18 Early Pregnancy Signs: Spotting Them and Confirming Your Pregnancy Sooner
Knowing you’re pregnant even before your period is due can bring peace of mind and the chance to start prenatal care right away. Within days of conception, subtle signals—from light spotting to shifts in your mood—can hint at a developing life. This guide covers 18 early pregnancy signs, explains how hormones like hCG and progesterone cause these changes, and tells you when to take a reliable pregnancy test or consult a women’s health expert. You’ll discover:
Follow Us!
- Which signs might appear before your missed period and how to tell implantation bleeding apart from your regular spotting
- The most common and the less obvious early signs that often go unnoticed
- When and how to take an early pregnancy test for the most accurate results
- The hormonal reasons behind these symptoms and the emotional shifts during early gestation
- Warning signs that require medical attention and ways to manage discomfort
What Are the First Signs of Pregnancy Before a Missed Period?
Early pregnancy symptoms can show up days before your menstrual cycle is expected, thanks to rising hormone levels that prepare your body for implantation. Light spotting, known as implantation bleeding, often happens 6–12 days after conception as the embryo settles into the uterine lining. Along with spotting, you might experience mild cramping, breast tenderness, fatigue, and slight changes in your body temperature. Recognizing these signals allows for timely confirmation with home or clinic-based testing and early prenatal appointments at a women’s health clinic offering caring, precise diagnostic services.
Which Early Symptoms Can Appear Before a Missed Period?
Before your period is due, you might experience a range of early signs as your symptoms of pregnancy and progesterone levels start to climb.
- Light spotting or a pinkish discharge within two weeks of conception
- Mild, twinge-like cramps that feel similar to menstrual discomfort
- Breast sensitivity or a feeling of fullness due to increased blood flow
- Fatigue, a result of elevated progesterone slowing your metabolism
- Slight increases in your basal body temperature, indicating hormonal shifts
Each of these signs is directly linked to implantation or hormone-driven changes, and noticing several symptoms together increases the likelihood of early pregnancy. Tracking your basal temperature and cervical mucus patterns can further support these observations and guide you on when to test.
These early clues naturally lead into understanding how implantation bleeding differs from a regular period.
How Does Implantation Bleeding Differ from a Period?

Implantation bleeding is typically lighter, lasts for a shorter time, and is less painful than menstrual flow.
| Characteristic | Implantation Bleeding | Menstrual Period |
|---|---|---|
| Volume | Spotting or very light discharge | Moderate to heavy flow |
| Duration | 1–2 days | 3–7 days |
| Color | Light pink to brown | Bright to dark red |
| Associated Cramping | Mild, brief twinges | Stronger, longer-lasting cramps |
Spotting often occurs without the full range of menstrual cramps and isn’t accompanied by significant shedding. Noticing these differences helps in recognizing early symptoms and leads to exploring the hormonal factors behind them.
What Hormonal Changes Cause Early Pregnancy Symptoms?
Human chorionic gonadotropin (hCG) and progesterone surge shortly after implantation, orchestrating the early pregnancy symptoms. hCG supports the corpus luteum to keep producing progesterone, while progesterone relaxes uterine muscles and boosts blood supply to the developing embryo. Estrogen also rises concurrently to support uterine growth and circulation. These hormonal shifts can manifest as nausea, breast tenderness, and mood changes. Understanding these processes helps explain why symptoms can vary in intensity and timing, and prepares you for when to seek reliable testing or expert advice at a women’s health clinic.
Biological Functions of Human Chorionic Gonadotropin (hCG) in Early Pregnancy and Implantation hCG stimulates progesterone production by corpus luteum cells; promotes angiogenesis in uterine vasculature; induces cytotrophoblast cell fusion and differentiation into syncytiotrophoblast cells; inhibits maternal immune responses, including macrophage activity, against placental cells; stimulates uterine growth commensurate with fetal growth; suppresses myometrial contractions throughout pregnancy; promotes growth and differentiation of the umbilical cord; signals the endometrium to prepare for implantation; acts on maternal brain receptors, leading to hyperemesis gravidarum, and appears to promote fetal organogenesis during pregnancy. Biological functions of hCG and hCG-related molecules, 1912.
How Can You Tell If You’re Pregnant Early Through Symptoms?
Early pregnancy symptoms can resemble premenstrual syndrome (PMS), but they often have distinct patterns and durations. By comparing symptom clusters, you can differentiate pregnancy signs from PMS and decide when to confirm with a test or a clinical evaluation.
What Are the Most Common Early Pregnancy Symptoms?
- Nausea or queasiness, often called morning sickness, caused by hCG stimulating nausea centers in the brain
- Fatigue, a side effect of progesterone’s sedative effect and increased blood volume
- Breast tenderness and swelling, due to estrogen and progesterone boosting glandular activity
- Frequent urination as the growing uterus presses on the bladder and kidneys work harder to filter fluid
- Mild cramping linked to the uterus expanding
These core signs indicate early gestational changes, prompting many women to seek home testing or in-clinic confirmation and initial prenatal counseling.
How to Differentiate Early Pregnancy Symptoms from PMS?
| Symptom Feature | Early Pregnancy | PMS |
|---|---|---|
| Breast Tenderness | Persistent, increasing sensitivity | Fluctuates, usually eases after period starts |
| Nausea | Can occur at any time of day | Rare |
| Fatigue | Intense, not easily relieved by rest | Often improves with sleep |
| Mood Swings | May include heightened anxiety or euphoria | Irritability, feelings of sadness |
| Spotting | Light implantation spotting, brief | Heavier flow, longer duration |
Pregnancy-related symptoms often continue or intensify rather than disappear once bleeding begins. Noting these patterns can help you decide whether to take an early pregnancy test or consult a women’s health clinic for diagnostic procedures.
Association Between Premenstrual Symptoms and Early Pregnancy Symptoms The overall severity of premenstrual symptoms was significantly associated with the overall severity of early pregnancy symptoms (b= 0.4, 95% CI = 0.3–0.5; p < 0.001). Early pregnancy symptom severity was most accurately predicted by the severity of premenstrual irritability. The most consistent predictor for a specific early pregnancy symptom was its corresponding premenstrual symptom. These associations between premenstrual and early pregnancy symptoms lend support to the reproductive hormone sensitivity hypothesis, suggesting that certain women may be predisposed to recurrently experiencing specific psychological and physical symptoms across different reproductive phases. Premenstrual symptoms are associated with psychological and physical symptoms in early pregnancy, HU Wittchen, 2013
What Are Less Common but Important Early Symptoms?
- A metallic taste in your mouth, caused by hormonal changes affecting taste perception
- A heightened sense of smell, due to estrogen making your olfactory pathways more sensitive
- Nasal congestion from increased blood flow to your nasal passages
- Headaches triggered by vascular changes from rising hormones
- Mild dizziness or lightheadedness as your blood pressure and sugar levels fluctuate
These less common symptoms add to the overall picture of early pregnancy and can guide personalized symptom management plans offered by a women’s health clinic.
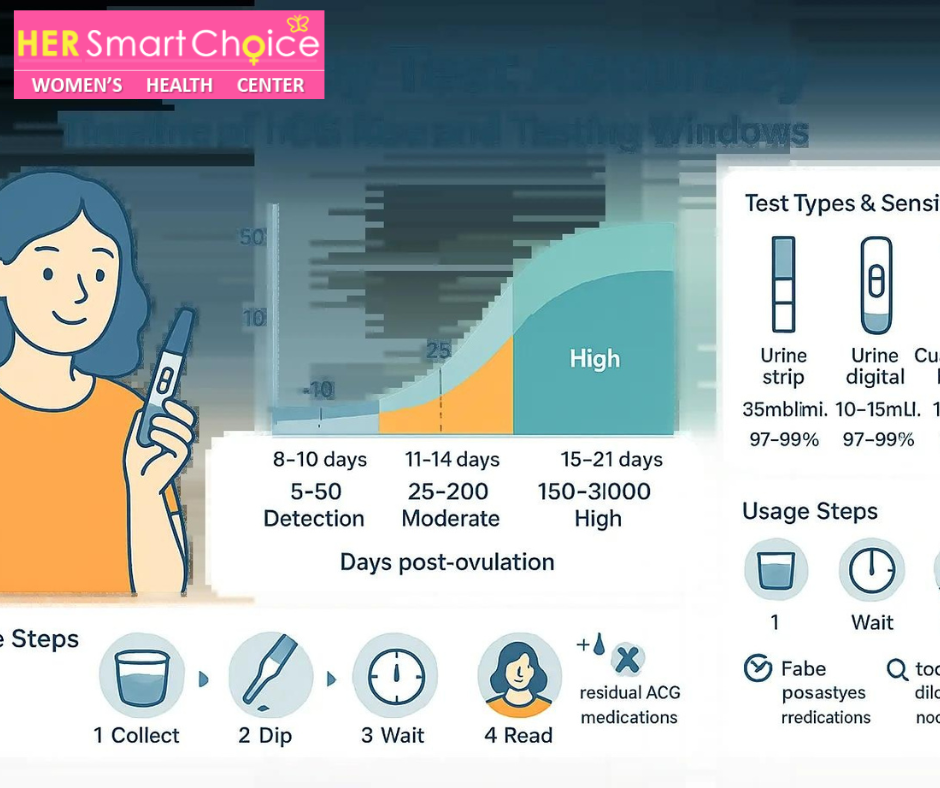
When and How Should You Take an Early Pregnancy Test?
Home and clinical tests detect hCG with varying sensitivity; the timing and type of test affect reliability. Testing too soon might lead to false negatives, while waiting until just after your missed period improves accuracy. Professional services at a women’s health clinic can include both urine and quantitative blood hCG testing for definitive confirmation and ongoing monitoring.
How Accurate Are Early Pregnancy Tests Before a Missed Period?
Early home pregnancy tests claim 76–96 percent accuracy when taken 3–5 days before a missed period. Accuracy increases as you get closer to your expected cycle date because hCG levels double every 48–72 hours. Blood tests performed in a clinic setting can detect lower hCG concentrations and confirm pregnancy with over 99 percent accuracy even before a missed period.
What Types of Pregnancy Tests Are Available?
- Urine-based home tests that detect hCG by showing color changes on a test strip
- Urine tests administered at a clinic with professional interpretation
- Quantitative blood tests that measure the exact hCG concentration
- Transvaginal ultrasound follow-up to visualize the embryo after hCG confirmation
Each diagnostic method is suited for different stages of early pregnancy. Consulting a women’s health clinic ensures test results are interpreted correctly and that follow-up care is arranged promptly.
When Is the Best Time to Take a Pregnancy Test for Reliable Results?
For the highest accuracy, take a home urine test using your first morning urine immediately after your missed period. If testing earlier, wait at least one week before your expected period date to allow hCG levels to reach detectable amounts. If results are still unclear, schedule a blood test or a telehealth consultation with a women’s health clinic, which can offer sensitive quantitative assays and expert guidance on your next steps.
Understanding testing strategies helps pave the way to exploring the hormonal influences behind these symptoms.
How Do Hormones Influence Early Pregnancy Symptoms?
Pregnancy hormones work together to help your body adapt to a growing embryo. Each hormone’s specific role explains why distinct symptoms appear and how they can be managed.
What Role Does hCG Play in Early Pregnancy?
Human chorionic gonadotropin (hCG) is produced by the developing placenta and supports the corpus luteum, which secretes progesterone essential for maintaining the uterine lining. Rising hCG levels can trigger morning sickness by stimulating the brain’s vomiting center and may cause breast tenderness as hormone receptors in glandular tissue swell.
This central hormonal connection sets the stage for progesterone and estrogen’s effects on energy and mood.
How Do Progesterone and Estrogen Affect Symptoms Like Fatigue and Mood Swings?
Progesterone relaxes smooth muscle tissue to prevent uterine contractions, but it also slows down the digestive tract and promotes drowsiness, leading to early pregnancy fatigue. Estrogen helps widen blood vessels, increase blood flow to the uterus, and regulate neurotransmitters, which can result in mood fluctuations and occasional anxiety. These combined hormonal actions explain why emotional and physical symptoms often appear together during the first trimester.
Connecting hormonal shifts to physical signs clarifies how implantation initiates another set of early indicators.
How Does Implantation Trigger Spotting and Cramping?
As the embryo embeds into the uterine lining, tiny blood vessels can break, causing light spotting that might last one to two days. At the same time, local prostaglandin release and uterine muscle adjustments can produce mild cramping sensations that differ from menstrual pain. Recognizing implantation-related discomfort as a natural early symptom can prevent unnecessary worry and guide you toward confirmatory testing.
After examining the biological drivers, the next focus is on the emotional and psychological adjustments during early pregnancy.
What Are the Emotional and Psychological Changes in Early Pregnancy?
Hormonal surges affect not only your physical systems but also your mental well-being. You might experience a range of emotions, from joy to anxiety, as your body adjusts to pregnancy. Identifying these changes and using coping strategies can support your emotional health during these critical early weeks.
How Do Hormonal Shifts Affect Mood and Emotions?
Rising estrogen and progesterone alter neurotransmitter activity in the brain, making you more susceptible to mood swings, irritability, and tearfulness. hCG fluctuations can intensify stress responses, making small concerns feel more pressing. Understanding these hormone-emotion connections empowers you to anticipate emotional shifts and seek timely support from mental health resources or prenatal counselors at a women’s health clinic.
Building resilience around mood changes helps you manage common emotional symptoms like anxiety and fluctuations.
What Are Common Emotional Symptoms Like Mood Swings and Anxiety?
Early pregnancy can involve:
- Sudden crying spells or irritability without clear reasons
- Increased worry about pregnancy outcomes or morning sickness
- Occasional feelings of being overwhelmed as your routine changes
- Heightened sensitivity to sensory input due to emotional lability
These emotional states often accompany physical symptoms, and recognizing their normalcy can encourage proactive coping measures rather than undue stress.
How Can Women Cope with Early Pregnancy Emotional Changes?
Practical strategies can support emotional stability in early pregnancy:
- Engage in gentle exercise like walking or prenatal yoga to boost endorphins
- Practice relaxation techniques such as deep breathing and mindfulness meditation
- Maintain open communication with partners, friends, or support groups
- Seek telehealth or in-person counseling through a women’s health clinic for professional guidance
Implementing these coping methods can ease anxiety and improve mood regulation, preparing you to discuss when to involve a doctor in your early pregnancy care.
When Should You See a Doctor for Early Pregnancy Symptoms?
Most early symptoms are normal, but certain warning signs require immediate medical attention. Timely evaluation at a women’s health clinic or via telehealth can protect both your health and the developing embryo’s.
What Are Warning Signs That Need Immediate Medical Attention?
Seek urgent care if you experience:
- Severe abdominal pain on one side, which could indicate an ectopic pregnancy
- Heavy vaginal bleeding or large clots, signaling a possible miscarriage
- Dizziness, fainting, or a rapid heartbeat, suggesting significant blood loss
- High fever or chills, pointing to an infection
Recognizing these red flags and getting prompt medical evaluation can prevent complications and ensure appropriate intervention.
How Can a Women’s Health Clinic Help Confirm and Manage Early Pregnancy?
A specialized clinic offers comprehensive early pregnancy care:
- Symptom assessment and personalized risk evaluation
- Sensitive urine and quantitative blood hCG testing
- Ultrasound imaging to confirm an intrauterine pregnancy
- Initial prenatal guidance on nutrition, supplements, and lifestyle
Access to coordinated diagnostic services and compassionate counseling provides a strong foundation for prenatal care.
When Is Telehealth Consultation Appropriate for Early Pregnancy Concerns?
Telehealth is ideal for:
- Interpreting early home test results and advising on next steps
- Managing mild nausea, fatigue, or mood fluctuations
- Scheduling in-person visits when warning signs appear
- Providing ongoing emotional support with minimal disruption to your daily life
Virtual visits ensure timely expert input without travel, making early pregnancy care more accessible. Telehealth platforms connect you seamlessly to clinicians who can arrange in-clinic diagnostics when needed.
How Can You Manage Common Early Pregnancy Symptoms?

Relief strategies focus on nutrition, lifestyle adjustments, and targeted remedies to ease discomfort while supporting prenatal health.
What Are Effective Ways to Manage Morning Sickness and Nausea?
To ease queasiness:
- Eat small, frequent meals rich in complex carbohydrates and lean protein
- Sip ginger tea or chew crystallized ginger to calm your digestive system
- Avoid strong odors and opt for bland snacks like crackers first thing in the morning
Implementing these dietary and behavioral changes can reduce nausea episodes and help maintain hydration and nutrient intake.
How Can You Alleviate Fatigue and Breast Tenderness?
Combat tiredness and discomfort by:
- Prioritizing rest and taking short naps throughout the day
- Wearing a supportive, well-fitting bra to minimize pain from breast swelling
- Incorporating iron-rich foods and staying hydrated to maintain energy levels
Gentle self-care and a focus on nutrition can boost energy and comfort, enhancing your overall well-being.
What Should You Know About Frequent Urination and Other Physical Changes?
Increased urinary frequency is due to your kidneys adapting and the uterus pressing on your bladder. To manage this symptom:
- Limit fluids before bedtime but maintain overall hydration throughout the day
- Practice pelvic floor exercises to strengthen bladder control
- Accept mild bloating and constipation as hormone-driven changes, and increase dietary fiber
Understanding these adaptations prepares you for further changes and highlights the importance of regular prenatal check-ups at a women’s health clinic.
Managing early symptoms effectively completes the overview and supports a confident transition into tailored prenatal care.
Early pregnancy symptoms can be subtle or intense, but recognizing patterns and seeking timely confirmation ensures a healthy start. A women’s health clinic offers expert testing, diagnostic clarity, and compassionate support from the earliest signs through ongoing prenatal guidance. By tracking symptoms, understanding hormone-driven changes, and adopting practical relief strategies, women gain confidence and control during the sensitive first weeks of gestation. Early detection and professional care are the cornerstones of a positive pregnancy journey.
Follow Us!