Vaginal Discharge: Understanding Normal, Abnormal, and STI-Related Symptoms with Treatment Options
Vaginal discharge is a normal physiological process that helps clear dead cells, maintain lubrication, and preserve a healthy vaginal microbiome. Understanding the difference between normal and abnormal vaginal discharge empowers individuals to recognize early warning signs of infection, including sexually transmitted infections (STIs), and to seek timely care. This guide explains what healthy discharge looks like across the menstrual cycle and life stages, lists hallmark features of abnormal discharge, and maps colors and odors to likely causes. It then reviews STIs that commonly cause discharge, summarizes current guideline-based treatments, and provides practical prevention tips and what to expect during a clinic visit. Readers will also find quick-reference tables and checklists to support self-monitoring and clear guidance on when to seek professional testing and treatment.
Follow Us!
Throughout, keywords like vaginal discharge, abnormal vaginal discharge, and STI testing Los Angeles are woven into evidence-focused explanations to help you act on symptoms with confidence.
What Is Normal Vaginal Discharge and How Does It Vary?

Normal vaginal discharge is a mix of cervical mucus and vaginal secretions that varies with hormones and serves protective and reproductive functions. This fluid helps keep tissues lubricated, supports beneficial lactobacilli, and changes predictably with cycle phase, sexual arousal, and pregnancy. Typical healthy discharge is usually clear to white, odor-free or mildly scented, and ranges from thin and watery to creamy depending on timing; pH remains slightly acidic to discourage overgrowth of pathogenic bacteria. Understanding these baseline patterns helps distinguish physiological changes from signs of infection, which are covered next to help you triage symptoms effectively.
What Are the Typical Color, Consistency, and Odor of Healthy Vaginal Discharge?
Healthy discharge is generally clear or white, varies in thickness, and has little to no strong odor. Around ovulation it becomes clear and stretchy, reflecting increased cervical mucus to support conception, while in the luteal phase it often appears thicker and creamier due to progesterone influence. Mild odor can be normal, but a sudden strong, fishy, or foul smell suggests an imbalance or infection. Keeping track of these typical characteristics makes deviations easier to spot and discuss with a clinician.
How Does Vaginal Discharge Change During Menstrual Cycle, Pregnancy, and Arousal?
Hormonal shifts drive predictable changes in volume and character of discharge across life stages and arousal. During the follicular phase discharge may be light and watery, peaking around ovulation with clear, elastic mucus; after ovulation it often becomes thicker and less copious. Pregnancy commonly increases overall volume due to elevated estrogen and blood flow, producing benign leukorrhea that is usually odorless; sexual arousal transiently increases lubricating secretions. Recognizing these physiologic patterns reduces unnecessary concern while highlighting when persistent or symptomatic changes need evaluation.
What Is Leukorrhea and When Is It Considered Normal?
Leukorrhea describes increased white or yellowish vaginal discharge and can be either physiological or pathologic depending on context. Physiologic leukorrhea occurs with ovulation and pregnancy and is typically odorless and not associated with irritation, whereas pathologic leukorrhea accompanies itching, burning, a strong odor, or atypical color and signals infection or inflammation. If increased discharge is accompanied by symptoms or persists beyond a few days, testing helps determine the cause and appropriate therapy. Monitoring duration and associated signs improves diagnostic accuracy at a clinic visit.
How Can You Recognize Abnormal Vaginal Discharge and Its Symptoms?
Abnormal vaginal discharge departs from your baseline in color, odor, texture, or accompanying symptoms, indicating infection or irritation that may require treatment. Key red flags include green or yellow discharge, a fishy smell, cottage-cheese texture with intense itching, sudden increase in volume with pelvic pain, or bleeding unrelated to menses. Differentiating among causes—bacterial vaginosis, yeast infection, irritant vaginitis, or STIs—relies on combining symptom clusters with risk factors and targeted testing. Early recognition and appropriate testing improve outcomes and guide effective treatment choices, which are summarized later.
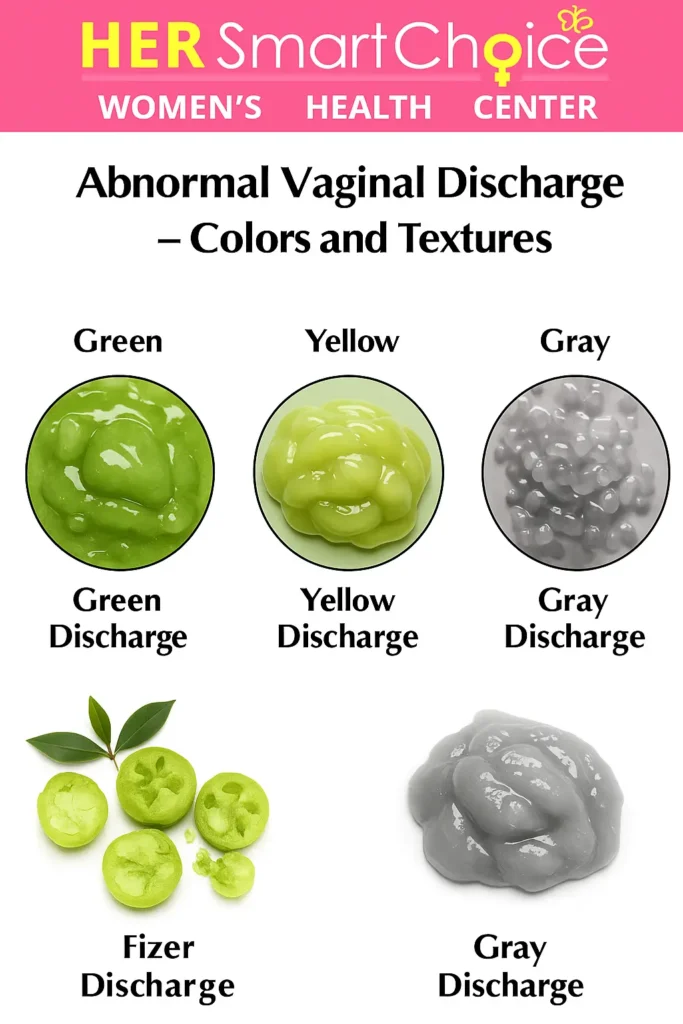
What Are the Key Signs of Abnormal Vaginal Discharge: Color, Smell, and Texture?
Abnormal discharge often presents with distinctive combinations of color, odor, and consistency that point toward specific conditions. Green or yellow frothy discharge commonly suggests trichomoniasis, gray and fishy-smelling discharge indicates bacterial vaginosis, and thick, white, curd-like discharge with pruritus is typical for yeast infection. Purulent, malodorous discharge accompanied by pelvic pain raises concern for STIs like gonorrhea or for ascending infection. Noting these key characteristics helps prioritize testing and management decisions.
This research highlights how specific symptoms and clinical findings can help identify the causes of vaginal discharge.
Identifying Etiologies of Vaginal Discharge: Symptomatology, Clinical Findings, and Diagnostic Performance Objective: To determine the diagnostic accuracy of various gynecologic symptoms and signs in identifying the causes of vaginal discharge. Method: Eighty-two subjects participated in this cross-sectional study. Gynecologic symptoms and signs were assessed for each subject, and laboratory examinations were performed to identify the etiology. The diagnostic accuracy of each symptom and sign was compared against laboratory examination as the reference standard. Symptoms and signs with a positive predictive value (PPV) greater than 50% were considered to have good diagnostic accuracy. Results: For bacterial vaginosis, excessive genital wetness, vulvar maceration, and thin, turbid, yellowish vaginal discharge demonstrated PPVs of 53%, 52%, and 52%, respectively. For candidal vaginitis, vulvar maceration and white, curd-like vaginal discharge had PPVs of 58% and 100%, respectively. For trichomoniasis, thin, turbid, frothy, yellowish vaginal discharge and strawberry cervix appearance Identifying Causes of Vaginal Discharge: The Role of Gynecologic Symptoms and Signs, D Ocviyanti, 2015
Which Symptoms Accompany Abnormal Discharge: Itching, Burning, Pain, and More?
Associated symptoms help distinguish localized vulvovaginal conditions from systemic or ascending infections. Itching and external irritation are classic for yeast infections or contact dermatitis, whereas burning with urination or pelvic pain may indicate urinary tract involvement or STIs. Fever, severe lower abdominal pain, or shoulder-tip pain suggests possible pelvic inflammatory disease (PID), which requires urgent evaluation. Recognizing clusters of symptoms supports timely triage and appropriate testing.
What Are Common Non-STI Causes of Abnormal Vaginal Discharge?
Several non-sexually transmitted conditions account for most abnormal discharge presentations and are managed differently than STIs. Bacterial vaginosis arises from disruption of lactobacilli dominance leading to a fishy odor and gray discharge, while candidiasis (yeast) causes intense itching and thick white discharge due to Candida overgrowth. Irritant or allergic vaginitis from soaps, douches, or scented products produces variable discharge and external irritation without infectious markers. Identifying non-STI causes avoids unnecessary antibiotic use and directs correct topical or oral therapy.
Which Sexually Transmitted Infections Cause Vaginal Discharge and What Are Their Symptoms?
Several STIs commonly cause vaginal discharge, each with characteristic but sometimes overlapping presentations that necessitate testing for accurate diagnosis. Chlamydia often produces minimal or mucopurulent discharge and may be asymptomatic; gonorrhea more reliably causes purulent yellow-green discharge with pelvic pain and systemic spread risk; trichomoniasis typically causes frothy greenish-yellow discharge with strong odor and vulvovaginal inflammation. Because symptom overlap is common and many infections are asymptomatic, laboratory testing is essential for confirmation and treatment planning. To educate women about normal vs. abnormal vaginal discharge, its link to sexually transmitted infections, and the latest STI treatment guidelines, helping readers recognize symptoms early and seek professional care at Her Smart Choice Women’s Health and Abortion Clinic in Los Angeles.
Understanding the clinical manifestations and treatment of Chlamydia trachomatis infection is crucial, especially given its prevalence and potential for asymptomatic presentation in women.
Chlamydia Trachomatis Infection: Clinical Manifestations, Diagnostic Approaches, and Therapeutic Strategies Chlamydia trachomatis infection predominantly impacts the urogenital system. In males, the infection typically presents with symptoms such as dysuria and penile discharge. Untreated chlamydial infections in men can lead to epididymitis. The majority of women infected with chlamydia exhibit minimal or no symptoms, although some may develop pelvic inflammatory disease. Neonatal chlamydial infections can result in ophthalmia neonatorum. Chlamydial pneumonia may manifest in infants aged one to three months, characterized by a gradual onset of a staccato cough, generally without wheezing or fever. Therapeutic regimens for uncomplicated urogenital infections include a single 1-gram oral dose of azithromycin or oral doxycycline at a dosage of 100 mg twice daily for seven days. Recommended treatment during pregnancy involves erythromycin base or amoxicillin. The Centers for Disease Control and Prevention and the U.S. Preventive Services Task Force advocate for screening for chlamydial infection in women at elevated risk. Diagnosis and treatment of Chlamydia trachomatis infection, 2006
Intro to table: The following comparison summarizes discharge features and common additional symptoms to help triage likely STI causes versus non-STI etiologies before testing.
| Condition | Discharge Characteristics | Other Common Symptoms |
|---|---|---|
| Chlamydia | Clear to mucopurulent, often scant | Dysuria, postcoital bleeding, often asymptomatic |
| Gonorrhea | Purulent yellow-green, moderate to heavy | Pelvic pain, fever, possible systemic spread |
| Trichomoniasis | Frothy green-yellow, strong odor | Vaginal itching, vulvar irritation, dyspareunia |
| Bacterial Vaginosis (non-STI) | Thin, gray, fishy odor | Minimal itching, altered pH |
What Are the Latest STI Treatment Guidelines and Available Options for Vaginal Discharge?
Current guideline recommendations prioritize evidence-based, single-dose or short-course regimens for common STIs, paired with partner management and follow-up testing when indicated. For trichomoniasis, metronidazole or tinidazole in recommended dosing remains first-line; chlamydia is treated with doxycycline as preferred oral therapy in many guidelines, and gonorrhea treatment centers on ceftriaxone-based regimens with adjunctive oral therapy per resistance patterns. Bacterial vaginosis is often managed with metronidazole orally or intravaginally, while candidiasis responds to topical or oral antifungals. Test-of-cure or retesting intervals depend on organism and local guidance with emphasis on treating recent partners to prevent reinfection.
To educate women about normal vs. abnormal vaginal discharge, its link to sexually transmitted infections, and the latest STI treatment guidelines, helping readers recognize symptoms early and seek professional care at Her Smart Choice Women’s Health and Abortion Clinic in Los Angeles.
Intro to table: The table below summarizes common conditions and first-line treatment options per current authoritative guidance for quick clinical reference.
| Condition/STI | Recommended First-Line Treatment | Notes & Follow-up |
|---|---|---|
| Trichomoniasis | Metronidazole or Tinidazole (per dosing guidelines) | Treat partner(s); symptomatic relief often rapid |
| Chlamydia | Doxycycline (oral, guideline-recommended) | Retest at 3 months in high-risk patients |
| Gonorrhea | Ceftriaxone-based regimen per updates | Test for co-infections and ensure partner therapy |
| Bacterial Vaginosis | Metronidazole oral or topical | Address risk factors; avoid douching |
What Are the Recommended Medications and Therapies for STI-Related Discharge?
Recommended medications target the identified pathogen and often include oral antibiotics or antiprotozoals with partner management strategies. For protozoal trichomoniasis, metronidazole or tinidazole remains effective for symptom resolution and microbial eradication, while bacterial STIs such as chlamydia and gonorrhea require organism-specific antibiotics with follow-up testing in selected cases. Non-STI infections like yeast respond well to azole antifungals administered topically or orally depending on severity and recurrence. Appropriate therapy reduces complications, transmission, and the likelihood of sequelae such as pelvic inflammatory disease.
How Does Her Smart Choice Women’s Health and Abortion Clinic in Los Angeles Provide STI Testing and Treatment?
Her Smart Choice Women’s Health and Abortion Clinic offers confidential, guideline-based reproductive health services including STI testing, counseling, and treatment tailored to patient needs in Los Angeles. Services include laboratory testing modalities appropriate for accurate diagnosis and clinician-directed prescriptions that follow current recommendations, plus counseling on partner notification and follow-up care. The clinic emphasizes accessible, women-focused options delivered with privacy and respect, supporting patients through treatment and prevention planning. For symptomatic individuals, seeking professional testing ensures correct diagnosis and avoids inappropriate self-treatment.
Also Read more: Vaginal Discharges: Types, Causes
When Should You Seek Professional Care for Vaginal Discharge Symptoms?
Seek professional evaluation when discharge deviates from your normal pattern or when red-flag symptoms appear, because timely diagnosis reduces complications and guides correct therapy. Urgent signs include severe pelvic pain, fever, heavy bleeding, or vomiting, all of which may indicate PID or another emergency requiring same-day care. Routine evaluation is warranted for persistent abnormal color or odor beyond 48–72 hours, new-onset painful urination, or symptoms after a new sexual partner. To educate women about normal vs. abnormal vaginal discharge, its link to sexually transmitted infections, and the latest STI treatment guidelines, helping readers recognize symptoms early and seek professional care at Her Smart Choice Women’s Health and Abortion Clinic in Los Angeles.
Red-flag checklist:
- Severe pelvic or lower abdominal pain: Seek immediate medical evaluation as this may indicate PID.
- Fever or chills with vaginal symptoms: Represents potential systemic infection and requires urgent care.
- Heavy, malodorous discharge with bleeding: Needs prompt assessment to rule out invasive infection or complications.
How Can You Maintain Optimal Vaginal Health and Prevent Abnormal Discharge?
Preventing abnormal discharge focuses on preserving the vaginal microbiome, practicing safe sex, and avoiding irritants that disturb native flora. Regular screening and vaccination where applicable, along with consistent condom use and prompt treatment of partners, reduce STI risk and recurrent infections. Avoiding douching, scented products, and ill-fitting synthetic underwear helps maintain an acidic pH and lactobacilli dominance that deter pathogenic overgrowth. These preventive strategies, combined with attention to systemic health factors like diabetes control and cautious antibiotic use, support long-term vaginal health.
What Are Essential Vaginal Hygiene Practices to Avoid Infection?
Simple hygiene practices preserve protective flora and reduce irritant exposure that can lead to abnormal discharge. Use gentle, unscented cleansers or plain water for external cleansing, avoid douching which disrupts pH balance, and choose breathable cotton underwear to limit moisture buildup. Change out of wet swimwear or sweaty exercise clothes promptly to prevent overgrowth of Candida and bacteria. These behaviors lower infection risk and make abnormal changes easier to detect when they occur.
List of hygiene dos and don’ts:
- Do wash externally with water and gentle, unscented soap.
- Don’t douche or use scented sprays and wipes in the vulvovaginal area.
- Do wear breathable fabrics and change out of wet clothing promptly.
How Do Safe Sex Practices Help Prevent STIs and Abnormal Discharge?
Consistent condom use, routine STI screening for sexually active individuals, and honest partner communication are cornerstone measures for preventing sexually transmitted causes of abnormal discharge. Vaccination against preventable infections reduces long-term risk, and prompt testing after new exposures limits onward transmission. Regular screening is particularly important because many STIs are asymptomatic yet can cause complications if untreated. Incorporating these practices into sexual health routines protects both partners and reduces the burden of infection-related discharge.
What Lifestyle Factors Can Influence Vaginal Discharge and Health?
Systemic factors such as recent antibiotic use, hormonal contraception changes, poorly controlled diabetes, and high stress can shift the vaginal ecosystem and influence discharge. Antibiotics can reduce lactobacilli and permit yeast overgrowth, while estrogen changes affect mucus production and consistency. Elevated blood glucose fosters Candida proliferation, increasing candidiasis risk, and stress may indirectly alter immune function and behavior that affect flora. Addressing modifiable factors—managing diabetes, discussing contraception effects with a clinician, and minimizing unnecessary antibiotics—helps stabilize vaginal health.
What Does the Vaginal Discharge Color Guide Reveal About Your Health?
A color-based approach to discharge helps prioritize likely causes but must be combined with odor, texture, symptoms, and risk factors for accurate interpretation. Clear or white discharge without irritation usually reflects normal physiology, while yellow or green discharge, especially with odor or itching, suggests infection. Gray discharge with a fishy smell is characteristic of bacterial vaginosis, and brown commonly reflects old blood or spotting rather than primary infection. A color chart is a practical monitoring tool when used alongside symptom tracking and clinical assessment.
Intro to color chart: The table below maps common discharge colors to likely causes and recommended actions to help you decide when to self-monitor versus seek testing.
| Discharge Color | Common Causes | Recommended Action |
|---|---|---|
| Clear | Normal (especially peri-ovulatory) | Monitor; seek care if persistent change occurs |
| White | Normal or yeast infection | If itchy, seek evaluation for candidiasis |
| Yellow/Green | Trichomoniasis or PID/STI | Seek testing; avoid self-treatment |
| Gray | Bacterial vaginosis | Test and treat per clinician guidance |
| Brown | Old blood, spotting | Monitor; seek care if accompanied by pain or odor |
What Does Clear, White, Yellow, Green, Gray, or Brown Discharge Indicate?
Each color tends to associate with specific conditions but must be interpreted in context of odor and symptoms. Clear discharge usually indicates normal lubrication or ovulation-related mucus, while white can be normal or indicate yeast if accompanied by intense itching. Yellow or green often points to infection such as trichomoniasis or an STI and merits testing. Gray plus fishy odor is strongly suggestive of bacterial vaginosis, and brown commonly reflects old blood or spotting rather than primary infection. Combining color with consistency and symptoms improves diagnostic likelihood.
When Does Discharge Color Signal an STI or Other Infection?
Discharge color raises STI suspicion when paired with risk factors and additional symptoms like pelvic pain, dysuria, or systemic signs. For example, green frothy discharge with a foul odor and new sexual exposure increases pre-test probability for trichomoniasis, while purulent yellow discharge with pelvic pain and fever warrants urgent STI testing. Conversely, color changes without symptoms and with stable risk profile may be benign and monitored. Testing is the only way to confirm an STI, so clinical evaluation should follow suspicious color-symptom combinations.
How Can You Use a Vaginal Discharge Color Chart to Monitor Symptoms?
A color chart works best when used consistently and documented with duration and associated symptoms to aid clinical assessment. Record the day, color, consistency, odor, and any accompanying symptoms, and bring this log to your appointment for efficient diagnosis. Use the chart as a screening tool rather than a diagnostic instrument; persistent or worsening changes should trigger testing. Sharing accurate notes with a clinician accelerates diagnosis and helps tailor guideline-based treatment.
How Can You Access Expert Care for Vaginal Discharge in Los Angeles?
Accessing expert care involves choosing a provider who offers confidential testing, evidence-based treatment, and supportive counseling for sexual and reproductive health. A typical visit includes history-taking, risk assessment, pelvic exam with specimen collection (swabs for NAAT, wet mount, pH), and a clear treatment plan with partner management recommendations when indicated. Expect clinicians to explain testing options, treatment rationale, and follow-up timelines while respecting privacy and patient autonomy. For residents in Los Angeles seeking local options, confidential and affordable reproductive health services are available that emphasize guideline-based care and follow-up.
What Services Does Her Smart Choice Women’s Health and Abortion Clinic Offer for Vaginal Discharge and STIs?
Her Smart Choice Women’s Health and Abortion Clinic provides confidential STI testing, laboratory-appropriate diagnostics, counseling, and treatment aligned with current clinical guidelines. Services include specimen collection for accurate testing modalities and clinician-directed prescriptions to treat infections and prevent complications. The clinic emphasizes patient-centered counseling on prevention, partner notification, and follow-up, delivered in a supportive environment for women-focused care in Los Angeles. These services help translate guideline recommendations into practical, timely treatment.
What Should You Expect During a Clinic Visit for Vaginal Discharge Evaluation?
A clinic visit typically begins with a focused sexual and medical history, followed by a pelvic exam to collect swabs and assess for visible signs of infection. Laboratory samples may include NAAT testing for STIs, microscopy for trichomonas or yeast, and pH testing to distinguish BV; results timelines vary by test type. After diagnosis, clinicians will explain treatment options, partner management, and follow-up or retesting plans as appropriate, aiming to reduce transmission and prevent complications. Clear communication about symptoms and risk factors enhances diagnostic accuracy and treatment effectiveness.
How Can You Book an Appointment for STI Testing and Vaginal Health Care in Los Angeles?
To book care, identify a provider offering confidential reproductive health services and prepare a brief symptom list and history of recent sexual exposures to streamline the visit. Bring identification and a list of current medications; be ready to discuss partner history and any recent antibiotic or hormonal changes that could affect diagnosis. Expect discretion and respect for privacy during scheduling and the visit itself, with clinicians focusing on guideline-based testing and individualized treatment plans. To educate women about normal vs. abnormal vaginal discharge, its link to sexually transmitted infections, and the latest STI treatment guidelines, helping readers recognize symptoms early and seek professional care at Her Smart Choice Women’s Health and Abortion Clinic in Los Angeles.
Appointment preparation checklist:
- List your symptoms and their duration.
- Note recent sexual partners or exposures.
- Bring any prior test results or medications.
This article has outlined how to recognize normal versus abnormal vaginal discharge, identified likely causes based on color and associated symptoms, summarized up-to-date treatment guidance, and described when and how to seek care. Early recognition, appropriate testing, and guideline-based treatment reduce complications from STIs and non-STI infections and protect reproductive health. To educate women about normal vs. abnormal vaginal discharge, its link to sexually transmitted infections, and the latest STI treatment guidelines, helping readers recognize symptoms early and seek professional care at Her Smart Choice Women’s Health and Abortion Clinic in Los Angeles.
Frequently Asked Questions
Maintaining optimal vaginal health involves several lifestyle changes. Eating a balanced diet rich in probiotics, such as yogurt, can support a healthy vaginal microbiome. Staying hydrated helps maintain mucosal health, while regular exercise promotes circulation. Additionally, managing stress through mindfulness or physical activity can positively impact hormonal balance. Avoiding irritants like scented soaps and douching is crucial, as these can disrupt the natural flora. Lastly, practicing safe sex and getting regular STI screenings are essential for preventing infections and maintaining overall reproductive health.
Hormonal fluctuations significantly influence vaginal discharge. During the menstrual cycle, estrogen levels rise and fall, affecting the quantity and consistency of discharge. For instance, around ovulation, increased estrogen leads to clear, stretchy discharge, which aids in conception. Conversely, during the luteal phase, progesterone causes discharge to become thicker and creamier. Hormonal contraceptives can also alter discharge patterns, sometimes leading to lighter or less frequent discharge. Understanding these changes helps individuals differentiate between normal variations and potential signs of infection or other health issues.
A balanced diet plays a vital role in maintaining vaginal health. Foods rich in probiotics, such as yogurt and fermented products, help support a healthy balance of bacteria in the vagina. Omega-3 fatty acids found in fish and flaxseeds can reduce inflammation, while antioxidants from fruits and vegetables support overall immune function. Staying hydrated is also essential, as it helps maintain mucosal health. Additionally, limiting sugar intake can prevent yeast overgrowth, which is linked to abnormal discharge. A nutritious diet contributes to overall reproductive health and well-being.
Yes, stress can significantly impact vaginal health and discharge. High stress levels can lead to hormonal imbalances, which may alter the normal patterns of vaginal discharge. Stress can also weaken the immune system, making individuals more susceptible to infections, including yeast infections and bacterial vaginosis. Furthermore, stress may affect sexual arousal and lubrication, leading to discomfort during intercourse. Practicing stress management techniques, such as mindfulness, yoga, or regular exercise, can help maintain hormonal balance and support overall vaginal health.
Several signs may indicate the need for STI testing. If you experience unusual discharge that is accompanied by a strong odor, changes in color, or a change in consistency, it’s essential to seek testing. Other red flags include itching, burning during urination, pelvic pain, or bleeding between periods. Additionally, if you have had unprotected sex or a new sexual partner, it’s advisable to get tested, even if you have no symptoms. Early detection and treatment of STIs can prevent complications and promote better reproductive health.
Tracking changes in vaginal discharge can be done effectively by maintaining a daily log. Note the color, consistency, odor, and any accompanying symptoms such as itching or burning. Record the timing of these changes in relation to your menstrual cycle, as this can help identify patterns. Using a color chart can also aid in visualizing changes and determining when to seek medical advice. Bringing this log to your healthcare provider can facilitate accurate diagnosis and treatment, ensuring you receive appropriate care based on your observations.
Follow Us!
Conclusion
Understanding vaginal discharge is essential for recognizing normal versus abnormal patterns, which can indicate underlying health issues or infections. By being informed about the characteristics of discharge and associated symptoms, individuals can take proactive steps towards their reproductive health. If you notice any concerning changes, don’t hesitate to seek professional evaluation and care at Her Smart Choice Women’s Health and Abortion Clinic in Los Angeles. Empower yourself with knowledge and take the next step towards maintaining optimal vaginal health today.