Vaginal Discharge After Abortion: What’s Typical, What’s Concerning, and When to Get Help
Vaginal discharge after an abortion is a normal part of healing: the uterus clears blood, tissue and mucus as it returns to its pre‑pregnancy state, producing different colors and textures over days to weeks. This guide explains what typical post‑abortion discharge looks like, how long common patterns usually last, and which changes suggest infection or other complications so you know when to seek care. At Her Smart Choice we aim to be a trusted medical resource — you’ll find a week‑by‑week view, practical monitoring steps, red‑flag lists, prevention and recovery tips, and concise answers to common questions about yellow or prolonged discharge. Recovery varies by procedure type and gestational age, so this article focuses on helping you spot healthy healing versus signs that need clinical evaluation, using clear examples, EAV‑style tables, and actionable checklists.
Follow Us!
What Is Normal Vaginal Discharge After an Abortion?
Normal post‑abortion discharge is usually a mix of fresh blood, older clots and vaginal mucus that gradually thins and lightens as the uterus heals. This reflects uterine involution and shedding of the decidua and residual blood — early bleeding tends to be red or brown, while mucus‑like or clearer discharge appears later to help clear debris and support tissue repair. Expect volume and color to decline over days to weeks; most people notice the heaviest bleeding in the first week and steady reduction afterward. Knowing typical colors and textures makes it easier to spot changes that could indicate infection or retained tissue, so the next section breaks down common appearances and timelines.
Typical colors and consistencies follow predictable stages: brown or dark red often represents older blood clearing out during the first 1–2 weeks, pink spotting appears as bleeding tapers, and mucus‑like or whitish discharge is common as the lining repairs. Mild or no odor is usual; a strong, unpleasant smell is not. These baseline patterns help you monitor changes and decide when to follow up with a provider.
Discharge usually decreases most quickly in the first 2–4 weeks, though intermittent spotting or brown staining can persist for some people up to 6–8 weeks. Duration varies with whether the abortion was medical or surgical, gestational age, and individual healing. If bleeding increases after initial improvement or heavy bleeding resumes, contact your clinician for reassessment. Below is a concise EAV‑style table summarizing common colors and what they commonly mean.
| Color / Type | Typical Consistency & Odor | Likely Meaning / Recommended Action |
|---|---|---|
| Bright red blood | Thin blood, occasional clots, minimal odor | Active bleeding common in the first few days; monitor volume and contact your provider if you’re soaking a pad in an hour |
| Brown or dark red | Thick, older blood, little to no odor | Normal as the uterus clears older blood; expect intermittent spotting for several weeks |
| Pink or light spotting | Thin, light flow | Normal as bleeding tapers; resume usual activities gradually as advised |
| Clear/white mucus | Watery or mucus‑like, odorless | Normal healing discharge that signals lining remodeling |
If your experience matches these patterns, healing is likely progressing. The next section explains how to recognize abnormal discharge and clear red flags that need prompt attention.
Common Colors and Consistencies Seen in Normal Recovery
Normal discharge typically starts bright red in the immediate days after the procedure, then shifts to brown and later to clearer, mucus‑like fluid as healing continues. Bright red usually means fresh bleeding from the uterine lining; brown indicates older blood being expelled. Later, whitish or clear mucus without a strong odor usually signals the cervix and uterus returning to baseline and often coincides with less cramping and lighter flow. Noticing these textures and colors helps you tell routine recovery apart from signs that need a clinical check.
Changes in consistency and color are influenced by hormones and the procedure type: some surgical procedures may show a faster drop in bleeding for some people, while medical abortions can cause longer spotting. If the discharge becomes thick, pus‑like, green or gray, or if you develop new systemic symptoms, treat it as potentially abnormal and see the section on infection signs below.
How Long Does Normal Discharge Last After an Abortion?
Most people have the heaviest bleeding in the first 1–3 days, with a noticeable reduction by 2–4 weeks and possible intermittent spotting that can last up to 6–8 weeks. The process reflects gradual uterine contraction and endometrial repair; larger gestations and retained tissue can prolong bleeding. Individual factors — clotting differences, prior infections, and the abortion method — affect timing, so use these timelines as general guidance rather than strict rules. A steady trend of improvement is reassuring; worsening color, increasing volume, or new symptoms should prompt evaluation. For more information, see our comprehensive guide on managing post-abortion bleeding.
Keep scheduled follow‑ups and communicate with your provider if you have concerns. Noting color, amount, smell and symptoms like cramping or fever makes triage faster and more accurate. If your recovery shows steady improvement, continue routine self‑care; if not, use the monitoring checklist later to prepare for a clinical call.
A simple self‑assessment framework helps patients track expected recovery patterns after abortion.
Post‑Abortion Care: A Framework for Patient Self‑Assessment The method compared outcomes of discharged post‑abortion patients to create self‑assessment tools that guide follow‑up and clarify common recovery responses.
How Can You Identify Abnormal Discharge and Signs of Infection After Abortion?
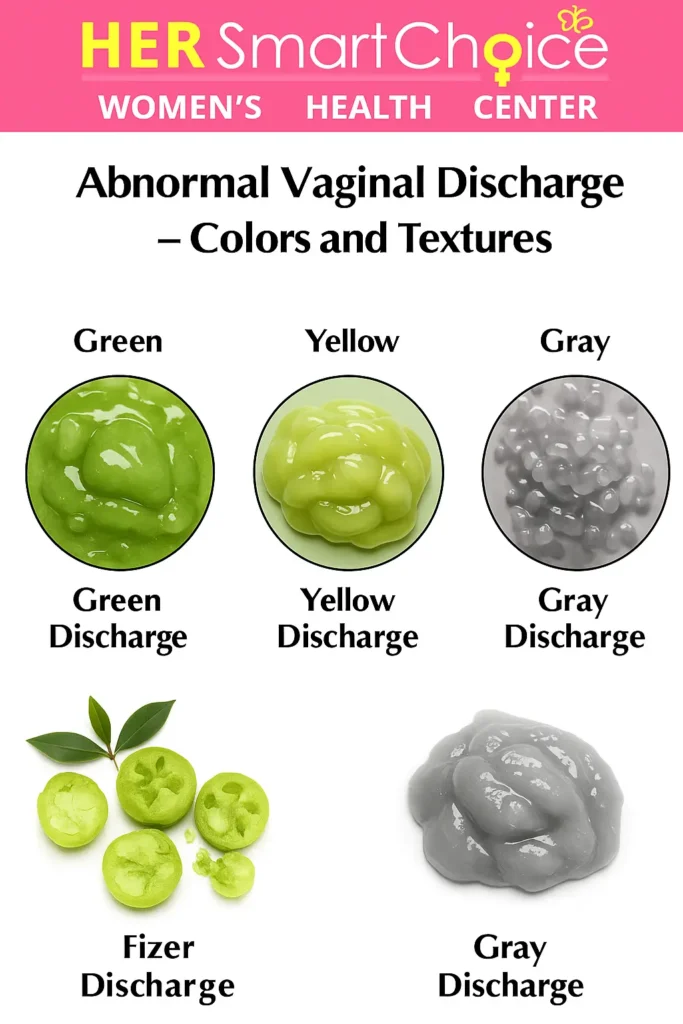
Discharge that is foul‑smelling, green or gray, thick and pus‑like, or accompanied by systemic symptoms such as fever or severe pain often indicates infection or retained tissue. Bacterial overgrowth or inflammation produces purulent material and can trigger systemic responses — these conditions usually need prompt clinical assessment and often antibiotics or a procedure. Early recognition of red flags improves outcomes and reduces the risk of serious complications like sepsis. The list below highlights the visual and systemic warning signs and the immediate actions to take. You can learn more about vaginal discharge for additional insights.
- Foul‑smelling vaginal discharge or a new, strong unpleasant odor — a sign of bacterial infection.
- Green, gray, or pus‑like discharge that is thicker than earlier mucus‑like drainage.
- New or worsening fever above 100.4°F (38°C), chills, or flu‑like symptoms suggesting systemic infection.
- Severe, continuous lower abdominal pain or heavy bleeding (soaking a pad in an hour) that could indicate retained tissue or hemorrhage.
These signs often appear together; for example, foul odor plus fever strongly suggests infection and needs urgent assessment. If you notice any combination of these symptoms, seek medical evaluation promptly — the next subsection describes how infected discharge typically looks and smells to help you decide when to call.
What Does Infected Discharge Look and Smell Like?
Infected discharge is commonly thick and discolored — yellow, green or gray — and usually has a noticeably foul or fishy odor, reflecting bacterial overgrowth or necrotic tissue. It may increase in volume and be accompanied by pelvic pain and tenderness. Typical causes include uterine infection from retained tissue or ascending bacteria after the procedure. Recognizing these visual and olfactory cues helps you prioritize medical contact when infection is suspected.
If infected discharge comes with systemic signs such as fever, chills or severe cramping, treat it as urgent and seek clinical care immediately. The following section lists other non‑discharge symptoms that often accompany infection and explains urgency levels for contacting a provider.
What Other Symptoms Indicate Post‑Abortion Infection?
Non‑discharge symptoms that commonly point to infection include fever over 100.4°F (38°C), persistent or worsening pelvic pain, dizziness or fainting, nausea or vomiting, and heavy bleeding with large clots. These signs reflect the immune system reacting to bacterial invasion or retained products of conception and can progress quickly without treatment. Use severity mapping: high fever, fainting, or heavy bleeding with signs of shock requires emergency care, while low‑grade fever or increasing pain usually warrants same‑day clinic evaluation. Monitoring symptom clusters and how they change helps decide whether to call your clinic or go to the emergency department.
Keep a brief symptom diary with temperature, pain level, bleeding amount and discharge details; this record helps clinicians triage and decide on interventions like antibiotics or further procedures. The next section groups discharge types and their most likely causes to help with decision‑making.
What Are the Different Types of Post‑Abortion Discharge and What Do They Mean?
Discharge can be grouped by color and consistency to suggest the most likely cause — from normal healing (brown or pink) to infection (green, gray, pus‑like) or retained tissue (heavy bleeding with clots). Underlying mechanisms include breakdown of blood products, mucosal repair, bacterial growth, or incomplete uterine evacuation. Mapping what you see to likely diagnoses helps target follow‑up and improves communication with clinicians. Below is an EAV‑style table pairing common appearances with probable causes and recommended actions.
| Appearance | Key Attributes | Differential Diagnosis / Recommended Action |
|---|---|---|
| Brown or dark red | Thick, older blood, low odor | Normal healing; monitor and follow up if persistent >8 weeks or if it worsens |
| Pink/light spotting | Thin, scant flow | Normal tapering bleeding; rest and routine monitoring |
| Yellow/green/gray | Thick, discolored, often foul odor | Possible bacterial infection; contact your provider for evaluation and likely antibiotics |
| Heavy bleeding with clots | Large volume, passing clots, dizziness | Possible retained tissue or hemorrhage; seek immediate medical care |
This mapping helps you decide when to monitor at home versus when to seek evaluation; act promptly if discharge suggests infection or if bleeding is heavy. The next subsections explain common normal colored discharge and when colored discharge becomes concerning.
What Does Brown or Pink Discharge After Abortion Mean?
Brown discharge usually represents older blood being expelled during uterine healing and is common in the first several weeks. Pink spotting is lighter and signals that fresh bleeding is tapering as the endometrium repairs. If these patterns are steady or improving, watch and wait is appropriate; but if brown or pink discharge comes with fever, worsening pain, or a sudden increase in bleeding, it could indicate retained products of conception or infection and should be evaluated. Tracking the trend and any associated symptoms helps decide whether clinical follow‑up is needed.
Is Yellow, Green, or Gray Discharge After Abortion a Cause for Concern?
Yellow, green or gray discharge is more likely to indicate infection when it is thick, persistent and has a foul odor, or when it is accompanied by fever or pelvic pain. Bacterial colonization or retained tissue can create purulent material and systemic symptoms that need antibiotics or procedural care. If such discharge appears but is mild, odorless and decreasing over 24–48 hours, close monitoring may be reasonable; any worsening or new systemic signs means contact your provider right away. Early treatment typically involves antibiotics aimed at common uterine pathogens and assessment (including ultrasound if indicated) to check for retained tissue.
The next section offers practical steps to reduce infection risk and support recovery after an abortion.
How Can You Prevent Infection and Support Healing After an Abortion?
Practical steps reduce the risk of post‑abortion infection by limiting bacterial exposure and supporting the body’s recovery. The basic idea is to avoid practices that introduce bacteria into the vagina or uterus, and to support immune function with good nutrition, rest and emotional care. Below are hygiene do’s and don’ts, lifestyle tips for recovery, and an evidence‑informed approach to emotional wellbeing.
Hygiene and activity guidance centers on avoiding intra‑vaginal products and keeping the external genital area clean and dry. The list below summarizes clear, actionable hygiene steps for recovery.
- Avoid intra‑vaginal products such as tampons, douches and menstrual cups until your provider clears you.
- Use sanitary pads rather than internal products and change them often to limit bacterial growth.
- Keep the external genital area clean and dry; wash gently with mild soap and water and avoid scented products or baths if your provider advises against them.
What Hygiene Practices Help Prevent Post‑Abortion Infection?
Avoiding douching, tampons and sexual intercourse for the provider‑recommended interval helps prevent ascending infections by keeping the cervical canal protected from external bacteria. Change pads frequently and wear breathable cotton underwear to reduce moisture that fosters bacterial growth. Practice careful hand hygiene before and after pad changes or personal care. If your clinician prescribes antibiotics or other instructions, follow them exactly. These precautions, combined with symptom monitoring, form the foundation of safe aftercare.
How Do Rest, Nutrition, and Emotional Well‑Being Support Recovery?
Rest and graded activity support uterine involution and can reduce bleeding; avoid heavy lifting and strenuous exercise in the immediate recovery period s/o your body can focus on repair. Nutrition — including iron‑rich foods, adequate protein and plenty of fluids — replenishes losses from bleeding and supports immune function. Sleep promotes overall healing and hormone balance. Emotional wellbeing matters because stress can heighten pain and slow recovery; reach out to friends, family or a counselor if you need support. Combining physical and emotional self‑care helps speed recovery and lowers the chance of complications.
Practical examples: gentle walking as tolerated after 24–48 hours, prioritizing iron and protein if bleeding was heavy, and contacting a clinician or support resources for persistent anxiety or depressive symptoms. The next section explains when to contact a doctor about discharge concerns, with clear warning signs.
When Should You Contact a Doctor About Discharge After an Abortion?

Contact a doctor when discharge is paired with systemic symptoms (fever, severe pain), when bleeding is heavy or getting worse, or when discharge becomes foul‑smelling, green/gray or pus‑like. These findings can signal infection, retained tissue or hemorrhage — conditions that may require antibiotics or immediate procedural care. Prioritizing these signs ensures timely treatment and lowers the risk of serious complications. The table below lists common symptoms, urgency levels and recommended immediate actions.
| Symptom / Finding | Characteristic | Urgency / Recommended Action |
|---|---|---|
| High fever (>100.4°F / 38°C) | Systemic sign, may include chills | Urgent: contact your provider right away or go to the ER if severe |
| Foul‑smelling or green/gray discharge | Thick, purulent odor | Urgent: contact the clinic same day for antibiotics and evaluation |
| Heavy bleeding (pad soaked in ≤1 hour) | Large volume, clots, lightheadedness | Emergency: go to the ER or call emergency services immediately |
| Mild spotting without fever | Light, decreasing flow | Routine: monitor and follow up at your scheduled visit |
This checklist clarifies which situations need emergency care versus same‑day clinic evaluation; acting according to these categories helps keep you safe. The next two subsections expand on absolute emergency signs and offer practical monitoring strategies for home use.
Warning Signs That Require Immediate Medical Attention
Seek emergency care for heavy bleeding that soaks a pad in an hour or less, passing very large clots, fainting or near‑fainting, sustained high fever above 100.4°F (38°C), or severe continuous abdominal pain not relieved by pain medication. These signs can indicate hemorrhage, sepsis, or retained tissue with acute infection and require immediate transport to an emergency department. Concrete examples — such as soaking two pads in an hour or feeling dizzy when standing — help you recognize severity quickly. If you have any of these signs, get emergency help without delay.
When you arrive, telling staff the amount of bleeding, how long you’ve had a fever, and whether you felt faint can speed triage and treatment. The following subsection gives a simple monitoring checklist to help you decide when to call your clinician before symptoms escalate.
How to Monitor Discharge Changes and Know When to Seek Help
A straightforward monitoring routine improves accuracy when assessing discharge and communicating with clinicians: note color, amount (light/moderate/heavy), odor, and associated symptoms like fever or pain, and record the date and time of any notable changes. If discharge worsens over 24–48 hours, if a new foul smell or green/gray color appears, or if systemic symptoms develop, contact your provider promptly — sooner if you have a fever or heavy bleeding. When calling, use concise phrases like: “I have green, foul‑smelling discharge for 12 hours and a fever of 101°F.” That helps clinicians triage correctly. Keeping a brief diary and using clear language speeds evaluation and improves care decisions.
Monitoring empowers you to act early and gives clinicians the information they need to recommend antibiotics, imaging, or in‑person assessment. The next section answers common patient questions about yellow discharge and prolonged bleeding.
Common Questions About Post‑Abortion Discharge
People often ask whether yellow discharge is normal and how long discharge can last. Short, evidence‑based answers help set expectations and reduce anxiety. The Q&A below gives direct guidance, clear qualifiers and sample phrases to use when contacting your clinician.
Is Yellow Discharge Normal After an Abortion?
Yellow discharge can be normal if it’s light, odorless and gradually decreasing — it may be old blood mixed with mucus as the lining heals. However, yellow discharge that is thick, foul‑smelling, or accompanied by fever or worsening pain is more likely to be an infection and needs prompt evaluation. If you’re unsure, monitor closely for 24–48 hours; any progression to a foul smell, a change toward green/gray, or new systemic symptoms should prompt a call to your provider. This approach balances reassurance for mild changes with clear escalation criteria for infection.
Can Discharge Last for Several Weeks After an Abortion?
Yes — intermittent spotting or brown discharge can continue for several weeks, sometimes up to 6–8 weeks, particularly after medical abortion or later gestations. This reflects ongoing uterine healing and gradual clearance of blood. Factors that prolong discharge include retained tissue, infection, and individual variation in uterine involution. Persistent worsening or new red‑flag symptoms should prompt evaluation. Track trends: steady improvement is reassuring, while increasing volume, a color change to green/gray, or new fever is not.
This guide gave practical timelines, visual cues, EAV‑style tables, prevention steps, monitoring checklists, and clear red‑flag criteria so you can tell normal recovery from issues that need care. Use the symptom descriptions and sample phrases here when contacting your clinician to help them assess urgency and plan next steps.
Frequently Asked Questions
If bleeding suddenly becomes heavier — especially if you’re soaking through a pad in an hour or less — seek medical attention immediately. This can indicate retained tissue or hemorrhage and may require urgent treatment. Watch for dizziness, severe pain or large clots, and call your healthcare provider or go to the ER right away if you have these signs.
Normal discharge typically includes blood, mucus and tissue that changes over time: bright red early on, then brown or pink, and later clearer or whitish. Abnormal discharge is often thick, foul‑smelling or green/gray and may come with fever or severe pain. Tracking color, odor and volume helps you identify concerning changes that warrant medical attention.
Mild cramping is common as the uterus contracts to heal and return to its pre‑pregnancy size. However, if cramping becomes severe, or occurs with heavy bleeding, fever or foul‑smelling discharge, contact your healthcare provider. Monitoring how intense and how long cramps last helps determine whether they’re within the expected range.
Support recovery with a balanced diet rich in iron and protein, plenty of fluids, and restful sleep. Avoid heavy lifting and strenuous exercise for a few days, use sanitary pads instead of tampons, and practice good hygiene. Emotional support — from friends, family or counseling — can also improve recovery and help manage stress or anxiety. For more information, check out our what to eat after abortion for fast recovery.
Track recovery by noting discharge color, consistency and volume, and any symptoms like cramping or fever. A simple diary with dates and brief notes is useful for discussions with your provider. Look for a gradual decrease in bleeding and improvement in symptoms; sudden changes or worsening signs should prompt medical advice. Keep follow‑up appointments as recommended.
Most providers recommend waiting at least two weeks before resuming sexual activity, or until your clinician clears you. This gives your cervix time to close and lowers infection risk. If you notice unusual discharge, pain, or other concerning symptoms, check with your provider before having sex. Talk openly with your partner about timing and comfort when you’re ready to resume intimacy.
Conclusion
Knowing the usual patterns of vaginal discharge after an abortion helps you recognize healthy recovery and identify possible complications. Monitor changes in color, consistency and associated symptoms so you can get timely care when needed. Empower yourself with this information and take practical steps to support healing. For more resources and guidance on post‑abortion care, explore our other articles and clinical resources.
Follow Us!