Abortion Pill vs. Surgical Abortion: Your Complete Guide to Choosing the Right Path
Deciding between the abortion pill and surgical abortion is a significant, time-sensitive choice influenced by how far along the pregnancy is, your medical background, what feels right for you, and what’s accessible. This guide breaks down medication abortion (the abortion pill) and surgical abortion, explaining how they work, who qualifies, and what to expect before, during, and after each option. Our aim is to help you make a well-informed decision. Many people look for clear comparisons on effectiveness, timing, privacy, recovery, and safety.
Follow Us!
This article offers evidence-based insights and practical checklists to help you talk with your healthcare provider. We’ll define medication abortion and the mifepristone-plus-misoprostol regimen, describe suction aspiration and dilation and evacuation (D&E) procedures, compare outcomes and recovery, and outline questions to ask your provider. The content includes current research and local care considerations for Los Angeles patients, all delivered with a compassionate, non-judgmental approach. By the end, you’ll have concrete facts, comparison tables, provider question lists, and local guidance to help you navigate your options and next steps.
What Is Medication Abortion and How Does the Abortion Pill Work?
Medication abortion, commonly known as the abortion pill, uses medications to end an early pregnancy. It works by blocking hormones essential for pregnancy and then causing the uterus to contract and expel pregnancy tissue. The standard approach involves taking mifepristone first, followed by misoprostol. These medications work together to detach and expel the pregnancy. This method is effective in early pregnancy and can be managed with telehealth or in-clinic support. Medication abortion offers a non-surgical choice that many patients prefer for its privacy and the ability to manage it at home, though clear follow-up is crucial to confirm it’s complete. Understanding the specific roles of each medication and the expected symptoms helps patients anticipate the timeline, manage side effects, and know when to seek medical attention.
What drugs are used in medication abortion: Mifepristone and Misoprostol?
Mifepristone and misoprostol are the two main medications used in medication abortion, each playing a distinct role in ending a pregnancy. Mifepristone works by blocking progesterone, which causes the uterine lining to break down and the pregnancy to detach. Misoprostol then stimulates uterine contractions to expel the pregnancy contents. Common side effects include heavy bleeding and cramping for several hours to days, nausea, and temporary fever or chills. Serious complications are rare but require prompt medical attention. Patients are screened for contraindications, such as certain medical conditions or concurrent medications, and providers explain the dosing schedule and what to expect during follow-up.
Mifepristone and Prostaglandin for Early Pregnancy Termination: Efficacy and Safety Combination therapy utilizing mifepristone and low-dose prostaglandin is presently employed in clinical practice for the termination of early pregnancy in China, France, Sweden, and the United Kingdom. This combined regimen is well-tolerated and demonstrates high efficacy, achieving a 95% rate of complete pregnancy terminations. Recent clinical investigations into pregnancy termination have centered on the dose optimization of mifepristone and the assessment of orally active prostaglandin derivatives. Clinical pharmacokinetics of mifepristone, O Heikinheimo, 1993
| Medication | How It Works | Typical Dosage/Timing |
|---|---|---|
| Mifepristone | Blocks progesterone; causes uterine lining breakdown and pregnancy detachment | One oral dose, followed by misoprostol 24-48 hours later |
| Misoprostol | Stimulates uterine contractions and expulsion | Taken orally, vaginally, or between the cheek and gum after mifepristone |
| Combined Regimen | Works sequentially for a medical abortion | Most effective up to the recommended gestational limit for medication abortion |
This table clarifies how these two medications work together and why timing is important for effectiveness and safety. Understanding the sequence helps patients anticipate expected effects and plan for follow-up.
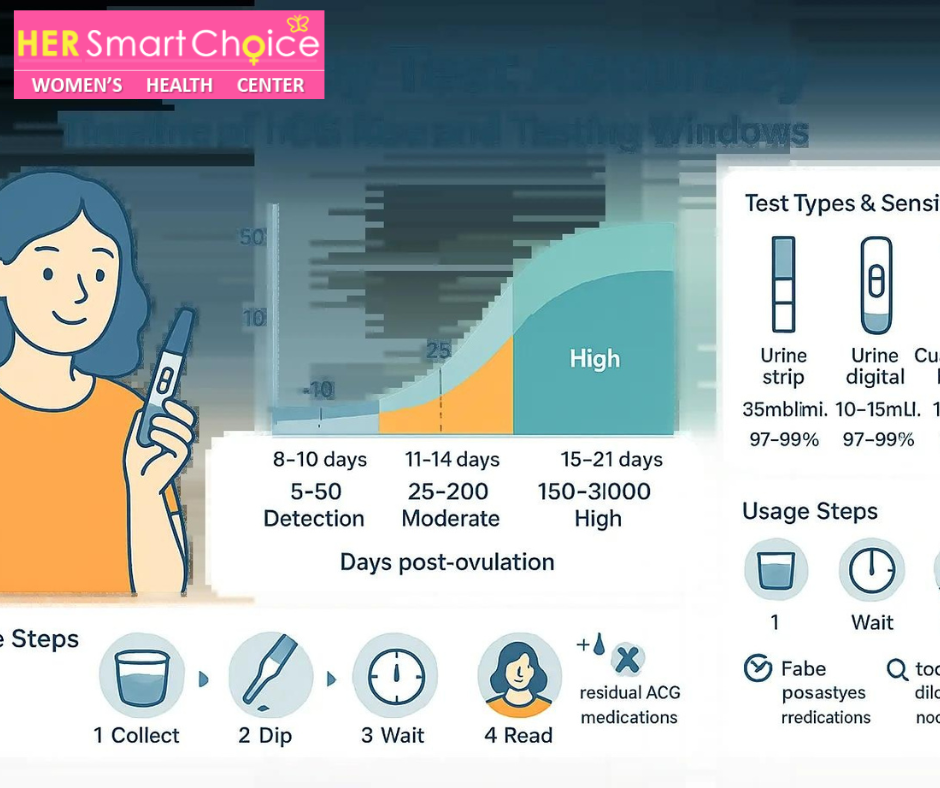
How does the medication abortion process unfold: timeline and symptoms?
The medication abortion process typically begins with a medical evaluation and decision, followed by taking mifepristone and then misoprostol 24–48 hours later. Active expulsion usually starts within hours after taking misoprostol. Most individuals experience significant bleeding and cramping during expulsion, often heavier than a typical period for several hours, gradually tapering over one to two weeks. Signs that the abortion is complete include reduced bleeding and a drop in pregnancy hormone (hCG) levels on follow-up tests. Persistent heavy bleeding, fever, or severe pain may indicate complications requiring prompt medical attention. Understanding this timeline helps patients prepare for pain management, rest, and follow-up arrangements.
Who is eligible for the abortion pill: pregnancy weeks and conditions?
Eligibility for medication abortion generally depends on how far along the pregnancy is. Many clinical guidelines support its use up to about 10 weeks of pregnancy, though exact limits can vary by provider and local regulations. Certain medical conditions, such as bleeding disorders, the use of specific blood-thinning medications, or an existing intrauterine device (IUD), might affect eligibility and require alternative approaches or extra precautions. A clinical assessment typically includes a review of your medical history, confirmation of gestational age (often via ultrasound), and a discussion about follow-up testing to ensure completion. It’s important to get evaluated promptly, as eligibility and effectiveness change as the pregnancy progresses.
What are the pros and cons of medication abortion?
Medication abortion offers several advantages that focus on patient comfort and control, alongside some trade-offs that influence the choice based on priorities like privacy, timing, and tolerance for bleeding. Key benefits include its non-surgical nature, the ability to manage much of the process at home, and broad accessibility through telehealth and pharmacy services in some areas. Downsides can include a longer active process with heavier bleeding and cramping for some hours or days, the necessity of reliable follow-up to confirm completion, and a small chance of needing a surgical procedure to finish. Considering these factors alongside your personal preferences helps you decide if medication abortion is the right fit for your needs.
- Key advantages include non-surgical care, the option for at-home recovery, and high effectiveness early in pregnancy.
- Notable disadvantages include prolonged bleeding/cramping, variability in symptom intensity, and occasional need for surgical follow-up.
- Access considerations include telehealth availability, local clinic policies, and the need for clear follow-up plans.
Overall, weighing the benefits of privacy and at-home management against potential prolonged symptoms helps guide the decision toward medication abortion or an in-clinic alternative.
How effective and safe is the abortion pill?
Medication abortion is highly effective when used within the recommended gestational limits. Early-regimen effectiveness is commonly reported in the mid-90% range, with effectiveness decreasing as gestational age increases. Major complications are uncommon. The most frequent clinical needs are for additional evacuation in cases of incomplete abortion or treatment for heavy bleeding, while severe infections or major hemorrhages are rare. Current research indicates that with appropriate screening, dosing, and follow-up, medication abortion is a safe option for many patients and is supported by professional guidelines. It’s important for patients to understand the context of success rates and the importance of follow-up testing or evaluation to confirm completion and manage any potential complications.
What Is Surgical Abortion and What Happens During an In-Clinic Procedure?
Surgical abortion refers to in-clinic procedures that physically remove pregnancy tissue using methods like suction aspiration (aspiration) or dilation and evacuation (D&E). These procedures are performed with appropriate anesthesia and clinical monitoring. They quickly evacuate the uterus using mechanical instruments and suction, with anesthesia and pain control options tailored to the gestational age and patient’s needs. Surgical abortion offers rapid completion, often a shorter active recovery period, and very high effectiveness. This may be why it’s recommended when immediate resolution is preferred or when medication abortion isn’t suitable. Understanding the procedural steps, anesthesia options, and recovery expectations helps patients prepare for the in-clinic experience.
What surgical methods are used: aspiration and dilation & evacuation?
Aspiration (suction) abortion is the most common method in early pregnancy. It uses gentle suction and instruments to remove uterine contents. Dilation and evacuation (D&E) is used later in the first trimester and into the second trimester. It combines dilation with instruments and suction to clear the uterus. Aspiration is typically used in early pregnancy and can often be performed with local anesthesia plus sedation if desired. D&E may require deeper sedation or general anesthesia and additional dilation time. Recovery expectations differ slightly by method; aspiration usually involves less time in the clinic, while D&E involves longer preparation and observation due to the gestational stage and anesthesia considerations.
| Method | Gestational Range | Anesthesia/Duration |
|---|---|---|
| Suction aspiration | Early first trimester | Local with sedation or moderate sedation; short procedure time |
| Dilation and evacuation (D&E) | Later first trimester to second trimester | Regional or general anesthesia possible; longer procedure and prep |
| Surgical evacuation (general) | Varies by clinical needs | Anesthesia choice tailored to patient and gestational age |
This table summarizes commonly used surgical approaches, showing how gestational age and anesthesia influence method selection and clinical logistics. Understanding these distinctions helps inform eligibility and scheduling.
Who qualifies for surgical abortion: gestational age and medical considerations?
Eligibility for surgical abortion depends on gestational age limits, cervical readiness, and specific medical factors that might favor a procedural approach, such as certain uterine abnormalities or contraindications to medication abortion. Providers determine suitability through a clinical evaluation that includes dating the pregnancy (usually by ultrasound), reviewing your medical history, and assessing risks related to anesthesia or bleeding disorders. Some patients are guided toward surgical care due to later gestational age, concurrent medical conditions, or a personal preference for quicker, in-clinic resolution. Pre-procedure counseling will cover expectations regarding anesthesia, recovery time, and follow-up.
What should patients expect during the surgical abortion procedure?
During a surgical abortion visit, patients typically undergo pre-procedure evaluation, provide consent, and may have cervical preparation before receiving anesthesia and undergoing the procedure itself. The actual aspiration or D&E step is usually brief, while the total clinic time includes recovery observation. Pain control is managed with local anesthetic, sedation, or general anesthesia, depending on the method and patient preference. Clinicians will provide instructions for post-procedure care, pain relief, and activity limitations. Most patients spend a few hours at the clinic and leave with clear follow-up plans and information on emergency signs to watch for. Knowing the sequence—pre-op, procedure, recovery—can help reduce anxiety and support planning for transportation and rest.
What are the advantages and disadvantages of surgical abortion?
Surgical abortion offers rapid, controlled completion with very high success rates and often less prolonged bleeding compared to medication abortion. Many patients value this predictability and shorter overall recovery. Downsides include the necessity of an in-clinic visit, potential use of anesthesia, a brief period of clinical observation, and logistical considerations like arranging transportation and time off work. Some patients prefer a procedural approach to minimize the uncertainty of at-home management, while others prefer medication abortion for privacy and to avoid anesthesia. Balancing speed and certainty against clinic access and anesthesia preferences helps many patients make their choice.
How safe and effective is surgical abortion?
Surgical abortion is among the safest common medical procedures. Effectiveness rates are typically in the high 90s percent, with low major complication rates when performed in appropriate clinical settings. Potential complications can include infection, retained tissue requiring repeat evacuation, or, rarely, heavy bleeding or uterine injury. Clinics follow strict protocols to minimize risks, including aseptic technique, appropriate anesthesia monitoring, and follow-up care. Patients are counseled on emergency signs and scheduled for routine follow-up when indicated. The high success and low complication profile make surgical abortion a reliable option in many clinical situations. For more information, you can read about the differences between surgical and medical abortion.
How Do Medication Abortion and Surgical Abortion Compare? Key Differences Explained
Comparing medication abortion and surgical abortion involves looking at effectiveness, timeline, privacy, recovery, cost, and access—factors that influence which method best suits a person’s needs. Medication abortion tends to offer more privacy and can be managed at home but involves a longer active process and heavier initial bleeding. Surgical abortion usually completes quickly in-clinic with less prolonged bleeding but requires a clinic visit and possibly anesthesia. Effectiveness is high for both methods when chosen within appropriate gestational windows, though surgical methods maintain slightly higher immediate completion rates in later pregnancy. Considering these trade-offs alongside availability, personal preferences, and medical history helps patients choose the method that best aligns with their priorities.
How do effectiveness rates differ between abortion pill and surgical abortion?
Effectiveness for medication abortion in early pregnancy is commonly reported in the mid-90% range. Suction aspiration and D&E have overall effectiveness in the high 90% range for complete uterine evacuation. Gestational age impacts effectiveness more significantly for medication abortion, with completion rates decreasing as pregnancy advances. Surgical methods, however, maintain consistently high success across broader gestational ranges. These differences mean medication abortion is highly effective for early pregnancy, but surgical options are often preferred when immediate, definitive completion is prioritized or when gestational age exceeds medication thresholds.
What are the timeline and duration differences for each abortion method?
Medication abortion typically unfolds over several days: initial clinical contact, mifepristone administration, misoprostol 24–48 hours later, and active expulsion within hours, followed by variable bleeding that may last one to two weeks. Surgical abortion usually involves a single clinic visit with preparation, a brief procedure, and several hours of recovery; bleeding and cramping generally subside more quickly. Follow-up timelines also differ: medication abortion commonly requires confirmation of completion by clinic visit or hCG testing within one to two weeks, while surgical abortion may have a shorter or optional follow-up depending on clinic practice.
- Medication abortion timeline: a multi-day active process, with bleeding lasting days to weeks.
- Surgical abortion timeline: a single-day procedure with shorter recovery and quicker resolution.
- Follow-up: medication abortion often requires more structured testing; surgical follow-up may be individualized.
These timeline contrasts inform logistics, time off work, childcare planning, and privacy considerations.
How do privacy and comfort levels compare between methods?
Medication abortion can offer greater privacy at home, as much of the process occurs outside the clinic, which some patients prefer for discretion and comfort. However, it requires managing heavy bleeding and cramping in a non-clinical setting. Surgical abortion provides a controlled clinical environment with onsite pain control and staff support, which can be more comfortable for patients who prefer immediate supervision and medical management. Comfort preferences vary: some patients value the privacy and autonomy of medication abortion, while others prioritize the predictability and shorter active discomfort of a surgical procedure.
What are the recovery times and aftercare needs for each option?
Recovery after medication abortion often involves heavier bleeding and cramping for the first 24–48 hours, tapering over one to two weeks, with recommendations for rest, hydration, and over-the-counter pain relievers. Surgical abortion recovery commonly allows a return to normal activities within a few days, with lighter bleeding and shorter overall downtime. Both methods require awareness of warning signs—fever, heavy soaking, severe pain—and prompt clinical follow-up. Contraception planning can begin immediately after both methods, and providers typically discuss options during follow-up or at the time of care.
How do costs and accessibility vary between medication and surgical abortion?
Costs and access depend on clinic pricing, insurance coverage, and the availability of telehealth or mailed medication options. Medication abortion may be more accessible through telehealth and mail in some regions, while surgical abortion requires clinic appointments and possible anesthesia resources. Insurance, local funding programs, and appointment wait times influence which option is feasible in a timely manner. Patients should explore funding assistance and local clinic resources to understand practical cost implications and scheduling availability for their situation.
How to Choose the Right Abortion Method: Factors to Consider
Choosing the right abortion method involves combining medical eligibility, gestational age, personal preferences for privacy and control, pain tolerance, logistical constraints, and emotional considerations into a decision framework. Patients should weigh the differences in timing and effectiveness, clinical contraindications, the need for follow-up, and how each option aligns with lifestyle needs, such as the ability to rest at home or take time for a clinic visit. A structured checklist and prepared questions for clinicians can empower patients to get clear, personalized guidance from a provider. Sound decision-making rests on matching clinical suitability with individual values and circumstances.
What role does gestational age play in choosing abortion type?
Gestational age is a primary determinant because medication abortion is most effective and commonly offered in early pregnancy, while surgical methods are available for later gestational ages and are sometimes required or preferred as pregnancy advances. Accurate dating—usually by ultrasound—is essential to determine eligibility and to select the safest, most effective method. As gestational age increases, options narrow, and some procedures may require different anesthesia or specialist referral, underscoring the importance of timely evaluation and scheduling.
How do personal preferences and medical history influence the choice?
Personal factors—such as a preference for at-home privacy, tolerance for bleeding and cramping, a desire for rapid completion, and comfort with anesthesia—directly shape method selection. Medical history elements, like bleeding disorders or certain medications that may contraindicate medication abortion, also play a role. Hypothetical scenarios can help patients map preferences to methods: someone prioritizing privacy and avoiding anesthesia might favor medication abortion early on, whereas someone needing quick resolution might prefer surgical care. Clinicians guide patients by applying medical criteria to these preferences to arrive at a safe, acceptable plan.
What questions should patients ask their healthcare provider?
Preparing targeted questions helps patients obtain the information needed to choose and plan care; a structured checklist ensures important topics are covered during the visit. Essential questions include eligibility based on gestational age and medical history, expected timeline and symptoms, pain control options, follow-up testing, potential need for additional procedures, contraception options after abortion, and logistics such as appointment timing and what to bring.
- Am I eligible for medication abortion or surgical abortion given my gestational age and medical history?
- What should I expect in terms of pain, bleeding, and recovery for each option?
- How will follow-up be handled, and how will we confirm the abortion is complete?
- What contraception options can I start immediately after the procedure or medication?
- What are the emergency signs that should prompt immediate care?
Using these questions during counseling ensures a shared decision-making process and prepares the patient for the next steps.
How does Her Smart Choice Women’s Health Clinic support compassionate decision-making?
Her Smart Choice Women’s Health Clinic in Los Angeles is dedicated to providing safe, factual, and compassionate guidance. We offer both medication abortion and surgical abortion as clinical options, along with patient-centered counseling to help individuals weigh trade-offs and make their decision. Our approach centers on evidence-based information, non-judgmental discussions about eligibility and personal priorities, and practical planning for follow-up care and contraception. Patients can expect individualized decision support that clarifies medical considerations and logistical steps without pressured recommendations, making informed choices easier during a stressful time.
What to Expect During Recovery and Aftercare for Both Abortion Methods?
Recovery and aftercare for medication and surgical abortion share core goals: manage pain and bleeding, detect complications early, and plan for contraception and emotional support as needed. Both methods require clear instructions for pain relief, activity restrictions, signs that need urgent evaluation, and appropriate follow-up testing or visits to confirm completion. Emotional responses vary and can include relief, sadness, or mixed feelings; clinics and support networks offer counseling resources to help patients process their experience. A structured aftercare checklist helps keep recovery on track and ensures prompt attention to any concerning symptoms.
What are the physical recovery timelines for medication vs surgical abortion?
Physical recovery after medication abortion usually involves intense cramping and bleeding for several hours, with decreasing bleeding over one to two weeks. Surgical abortion often results in shorter, more predictable bleeding and the ability to resume normal activities within a few days. Return-to-work timelines depend on individual recovery and job demands, and patients are advised to avoid heavy lifting or intense exercise for a short period. Full resolution of symptoms may take up to several weeks for some patients, and scheduled follow-up or hCG testing confirms completion when recommended.
How can patients manage pain and side effects after abortion?
Effective pain management includes over-the-counter pain relievers like ibuprofen or acetaminophen, using heat packs, resting, staying hydrated, and planning for time off for recovery. Clinics provide guidance on dosing and when prescription pain medication might be appropriate. Non-pharmacologic strategies like positioning, relaxation techniques, and pacing activities complement medications and support comfort. Patients are instructed to seek immediate medical attention for fever, soaking through multiple pads per hour, or severe, uncontrolled pain, as these signs may indicate infection or hemorrhage.
What emotional support resources are available post-abortion?
Emotional support options include clinic-based counseling, referrals to mental health professionals, peer support groups, and national or local helplines that offer confidential assistance. These resources can help process a range of feelings after an abortion. Providers routinely screen for emotional distress and can connect patients to tailored services when needed. Seeking support is an important part of aftercare, and patients are encouraged to communicate concerns with their clinician as part of comprehensive recovery planning.
What follow-up care is recommended after each abortion method?
Follow-up care for medication abortion often includes a clinic visit or hCG testing within one to two weeks to confirm completion. Surgical abortion follow-up may be individualized with an optional visit unless symptoms indicate otherwise. Both methods include counseling about contraception and the timing for initiation; many contraceptive options can be started immediately following the procedure or confirmed during follow-up. Clear instructions for emergency signs and accessible contact pathways for questions are essential elements of aftercare plans.
- Aftercare checklist includes pain control plan, signs of complications, contraception discussion, and scheduled follow-up.
- Patients should have a clear contact route for urgent concerns and a plan for emotional support as part of recovery.
- Confirming completion and preventing future unintended pregnancy are core goals of post-abortion care.
These aftercare steps ensure safe recovery and effective long-term reproductive planning.
What Are Common Questions About Abortion Pill and Surgical Abortion?
Patients frequently ask concise, practical questions about differences, safety, timing, side effects, and eligibility. Short, direct answers help capture key information for quick decision-making and provider discussions. The following answers provide focused facts that clarify core distinctions and expectations between medication and surgical abortion. Use these as conversation starters with a clinician to obtain personalized guidance.
What is the difference between medical and surgical abortion?
Medical abortion uses medication (mifepristone plus misoprostol) to end an early pregnancy and is often managed at home. Surgical abortion is an in-clinic procedure (such as suction aspiration or D&E) that physically removes pregnancy tissue. Medical abortion typically involves a multi-day process with heavier bleeding and cramping, whereas surgical abortion usually completes quickly in a clinical setting with anesthesia and shorter recovery. Choosing between them depends on gestational age, medical history, personal preferences for privacy and timing, and access to follow-up care.
Which abortion method is safer?
Both medication and surgical abortion are very safe when provided in appropriate clinical settings, with low major complication rates and high effectiveness for recommended gestational windows. Relative differences include slightly higher immediate completion rates for surgical methods in later pregnancy and more prolonged bleeding with medication abortion, but serious adverse events are uncommon for both. The safety of either option depends on proper clinical screening, timely follow-up, and access to medical care if complications arise.
How long does each abortion method take?
Surgical abortion usually takes place in a single clinic visit with a short procedure time and a few hours of total clinic stay, including recovery, allowing a return to normal activities within days. Medication abortion unfolds over multiple days: initial medication, follow-up dosing, active expulsion hours after misoprostol, and variable bleeding that may last up to one or two weeks. Follow-up timing also differs, with medication abortions more likely to require scheduled hCG testing or a visit to confirm completion.
What are the side effects of abortion pills?
Common side effects of abortion pills include heavy bleeding, cramping, nausea, vomiting, diarrhea, fever or chills, and temporary fatigue. Bleeding is often heavier than a regular period during the expulsion phase and then tapers. Serious but rare side effects include severe hemorrhage, ongoing incomplete abortion requiring surgical completion, or infection. Patients are advised to seek urgent care for fever lasting more than 24 hours, soaking multiple pads per hour, or severe, uncontrolled pain. Clear instructions on when to seek help are provided with the medication and during counseling.
When can you have a medical abortion versus a surgical abortion?
Medical abortion is typically offered in early pregnancy up to a provider-specific gestational cutoff (commonly around 10 weeks) and depends on clinical screening. Surgical abortion is available across broader gestational windows and may be required at later stages. Ultrasound dating and clinical evaluation determine eligibility for either method, and timely access is important because options change as gestational age increases. Telehealth and mailed medication pathways may expand access for medication abortion in some settings, subject to local regulations and clinician protocols.
Where to Find Safe and Compassionate Abortion Care in Los Angeles?
Finding safe, compassionate abortion care involves identifying clinics that provide evidence-based counseling, clear logistics for appointments and follow-up, and options that match clinical eligibility and personal preferences. Local care navigation helps with scheduling, understanding available services (medication vs. surgical), and arranging practical supports like transportation or funding referrals. Clinics that emphasize non-judgmental counseling and patient education help individuals make informed choices and prepare for both the clinical and emotional aspects of care.
What services does Her Smart Choice Women’s Health Clinic offer for abortion care?
Her Smart Choice Women’s Health Clinic offers comprehensive abortion care, providing both medication abortion and surgical abortion options, along with counseling and follow-up services to support decision-making and recovery. The clinic emphasizes safe, factual information and helps patients understand eligibility, expected timelines, pain management options, and contraception planning. Ancillary services include supportive counseling and coordination of follow-up testing as needed, ensuring patients receive a full continuum of care tailored to their clinical and personal needs.
How does the clinic ensure safe, factual, and non-judgmental guidance?
The clinic focuses on evidence-based counseling that explains medical indications, gestational age limits, and what to expect for each option, while respecting patients’ preferences and privacy. Staff provide clear informed-consent discussions, practical aftercare instructions, and referrals for emotional support or additional services when needed. This patient-centered approach helps individuals weigh medical facts alongside personal priorities and ensures follow-up plans are in place for safety and peace of mind.
How to schedule an appointment or consultation at Her Smart Choice?
To schedule care, patients typically contact the clinic to request an appointment or consultation. Clinical staff will then discuss eligibility questions, options, and outline any necessary pre-visit steps, such as ultrasound dating or medical history review. Preparing questions in advance, understanding the need for possible follow-up testing, and arranging transportation or support for the visit helps the process go smoothly. The clinic’s scheduling process aims to be responsive and supportive so patients can access timely, confidential care.
What local resources and support networks are available for abortion patients?
Local and national resources can assist with counseling, financial support, transportation, and additional referrals. Clinics commonly provide tailored local referrals and information on organizations that help with access barriers. Patients should ask their provider about community supports, peer groups, and mental health resources that fit their needs. Reaching out to a clinic for personalized referrals helps connect patients to the most current local services and supportive networks.
For individuals seeking local consultation or care, Her Smart Choice Women’s Health Clinic is presented as a compassionate Los Angeles resource that offers both medication abortion and surgical abortion with evidence-based counseling and follow-up support. If you are weighing your options, preparing the provider questions listed above and contacting a clinic for timely evaluation helps ensure safe, informed care and access to aftercare and emotional resources.
Frequently Asked Questions
Choosing an abortion method can bring up a range of emotions, including relief, sadness, or anxiety. It’s important to acknowledge these feelings and seek support if needed. Many individuals benefit from counseling or support groups to process their experiences. Emotional responses can vary widely based on personal beliefs, circumstances, and the method chosen. Clinics often provide resources for emotional support, and discussing feelings with healthcare providers can help in navigating this complex decision.
Preparing for your appointment involves gathering relevant medical history, understanding your menstrual cycle, and knowing your gestational age. It’s helpful to write down any questions you have about the procedures, potential side effects, and aftercare. Consider discussing your preferences for privacy, pain management, and recovery. Bringing a support person can also provide comfort and help you remember important information. Being prepared can lead to a more productive and reassuring consultation.
If you experience complications such as heavy bleeding, severe pain, fever, or any other concerning symptoms after an abortion, it is crucial to seek medical attention immediately. Complications, while rare, can occur and may require prompt evaluation and treatment. Having a clear understanding of emergency signs and knowing how to contact your healthcare provider can ensure timely care. Always follow the aftercare instructions provided by your clinic to minimize risks.
Aftercare for medication abortion typically involves managing heavier bleeding and cramping for several days, with follow-up appointments to confirm completion. In contrast, surgical abortion usually results in lighter bleeding and a quicker return to normal activities. Both methods require monitoring for signs of complications and discussing contraception options. Patients should follow specific aftercare instructions provided by their healthcare provider to ensure a safe recovery and address any concerns that may arise.
Insurance coverage for abortion services varies widely depending on the provider, state laws, and individual insurance plans. Some plans may cover the full cost of both medication and surgical abortions, while others may have limitations or require out-of-pocket expenses. It’s advisable to contact your insurance provider to understand your coverage options and any potential costs. Many clinics also offer financial counseling and can assist with navigating insurance claims or finding funding resources.
Many organizations provide financial assistance for abortion care, including local clinics, national funds, and non-profit organizations. These resources can help cover costs related to the procedure, travel, and other associated expenses. Patients should inquire at their clinic about available funding options and local resources. Additionally, some online platforms and hotlines can connect individuals with financial assistance programs tailored to their needs, ensuring access to necessary care without financial burden.
Follow-up care after an abortion is essential to ensure that the procedure was successful and to monitor recovery. For medication abortion, a follow-up visit or hCG testing is typically scheduled within one to two weeks to confirm completion. Surgical abortion follow-up may vary based on individual circumstances but often includes a check-in to discuss recovery and contraception options. Patients should be aware of signs that require immediate medical attention and maintain open communication with their healthcare provider during recovery.
Follow Us!
Conclusion
Choosing between medication abortion and surgical abortion involves understanding the unique benefits and considerations of each method, ensuring informed decision-making. This guide provides essential insights into effectiveness, recovery, and personal preferences, empowering individuals to navigate their options confidently. For personalized support and compassionate care, consider reaching out to Her Smart Choice Women’s Health Clinic for a consultation. Take the next step in your reproductive health journey today.