Warning Signs of Infection After Abortion: Key Symptoms and When to Seek Care
Infection after an abortion happens when bacteria grow inside the uterus or nearby tissues following a medical or surgical procedure. Recovery varies: many people have expected bleeding and cramping that ease over days to weeks. This guide helps you tell routine recovery from infection and shows when to get medical care. You’ll find the most common warning signs, clear thresholds you can measure at home (for example, fever ≥100.4°F / 38°C or soaking pads), how symptoms may differ by procedure type, possible complications, and practical next steps for urgent care. The thresholds and recommendations here follow standard public-health guidance so you can act quickly and safely.
Follow Us!
Most common warning signs of post-abortion infection
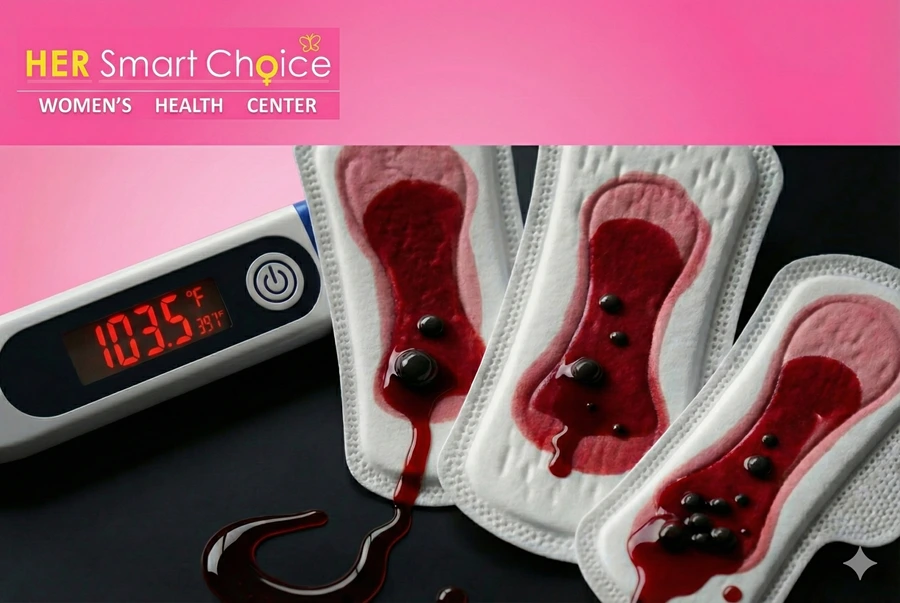
Post-abortion infection usually causes a mix of local uterine symptoms and systemic signs. Bacteria on retained tissue or introduced during a procedure can trigger inflammation, fever, and abnormal bleeding or discharge. Watch for measurable red flags that separate everyday recovery from infection: fever ≥100.4°F (38°C), bleeding that soaks many pads quickly, or a foul-smelling discharge. Catching infection early matters because untreated uterine infection can lead to endometritis or sepsis. Below is a short symptom list you can monitor at home, followed by a quick-reference table linking each sign to what to look for and what to do next.
Symptoms to watch for after an abortion include:
- Fever of 100.4°F (38°C) or higher, especially if it won’t go away or comes with chills.
- Heavy bleeding that soaks 2 or more pads per hour for two straight hours.
- Foul-smelling vaginal discharge or gray/green tissue-like material.
- Severe pelvic pain that gets much worse or won’t ease with your usual pain medicine.
- Systemic signs like a fast heartbeat, lightheadedness, or fainting.
These signs suggest possible infection; the sections that follow explain each one and why it matters.
Quick-reference table: core symptoms, measurable thresholds, and the recommended action if you see them.
| Symptom | Measurable Sign / Threshold | Recommended Action |
|---|---|---|
| Fever | Temperature ≥100.4°F (38°C), or persistent low-grade fever >48 hours | Call your provider the same day; seek urgent evaluation if you have chills or a very fast heartbeat |
| Heavy bleeding | Soaking ≥2 pads/hour for ≥2 hours or passing large clots >2 inches | Go to the emergency department or urgent care |
| Foul-smelling discharge | Strong, unpleasant odor; green/gray discharge or tissue-like clots | Contact your provider promptly for exam and possible antibiotics |
| Severe pelvic pain | Increasing pain not controlled by prescribed analgesics or sudden severe pain | Seek immediate in-person assessment; imaging may be needed |
| Systemic signs | Lightheadedness, rapid heart rate >100 bpm, low BP symptoms | Treat as possible sepsis—call emergency services |
If more than one of these signs appears, get care right away. The next sections explain each symptom in plain language and what it usually means.
How fever after abortion can signal infection
A fever after an abortion can mean your body is fighting an infection. A single temperature ≥100.4°F (38°C) or a fever that lasts more than 48 hours is concerning for bacterial infection rather than a normal inflammatory response. Accompanying symptoms—rigors, severe body aches, or worsening pelvic pain—raise the chance that the uterus is infected (endometritis). Retained tissue or bacteria introduced during a procedure can trigger this response. If your fever meets these thresholds or comes with other warning signs, contact your healthcare provider right away; antibiotics are often needed.
This leads into bleeding, which is another key measurable sign.
When heavy bleeding is a concern
Some bleeding after an abortion is expected as the uterus sheds tissue, but it becomes dangerous when it meets specific measurable criteria. If you’re soaking two or more standard pads per hour for two consecutive hours, passing clots about the size of a lemon or larger, feeling dizzy, or fainting, get emergency care. Heavy bleeding can happen with infection if products of conception are retained, but it can also indicate a separate urgent problem that needs immediate stabilization. If you meet these metrics or feel faint or lightheaded, go to the ER.
Knowing how to describe bleeding clearly helps when you call for help.
What foul-smelling discharge usually means
A strong, unpleasant vaginal odor—especially gray-green discharge or tissue-like material—often points to bacterial overgrowth or necrotic retained tissue in the uterus. Normal post-procedure bleeding may be brown or red with small clots and no strong smell. When the discharge is noticeably foul or changes color, it suggests infection such as endometritis. If you notice this, especially with fever or worsening pain, contact your provider for evaluation and likely antibiotics.
Changes in discharge often lead providers to examine you and consider imaging.
How to tell if abdominal pain and cramping suggest infection
Cramping and discomfort are normal after both medical and surgical abortion. Pain that steadily worsens, becomes sharp and localized, or doesn’t respond to usual pain medicines may signal infection or retained tissue. Infection-related pain is often constant, gets worse over time, and can come with fever or nausea. Localized tenderness or rebound pain may prompt an ultrasound to check for retained tissue or an abscess. Stop strenuous activity, take pain medicine as directed, and call your provider if the pain increases or comes with other warning signs.
Knowing the difference between expected cramping and concerning pain makes it easier to get care when needed.
Other systemic symptoms that suggest infection
When symptoms go beyond the pelvis, infection may be spreading. Watch for chills, persistent nausea or vomiting, a fast heart rate, dizziness, fainting, confusion, or low urine output—these can mean sepsis or serious systemic infection. If uterine symptoms occur alongside any of these signs, seek emergency care right away. Treatment for spreading infection usually includes IV antibiotics and close monitoring, so quick action is important.
Next, we explain how warning signs differ between medical and surgical abortion.
How warning signs differ between medical and surgical abortion
Warning signs vary by procedure because medical abortion uses medication over days to expel tissue, while surgical abortion is completed in clinic in one visit. Medical abortion often causes heavier bleeding and stronger cramping initially; infection risk rises if tissue is incomplete. Surgical abortion tends to have shorter, immediate bleeding and cramping after the procedure but carries a peri-procedural infection risk if bacteria are introduced or fragments remain. Comparing expected timelines and red flags helps you know what’s normal and what needs medical attention.
Below is a comparison table summarizing typical timelines and when symptoms suggest infection for each abortion type.
| Abortion Type | Typical Timeline / Expected Symptoms | When Symptoms Suggest Infection |
|---|---|---|
| Medical abortion (mifepristone + misoprostol) | Bleeding/cramping peaks within 24–72 hours, tapering over 1–2 weeks | Continued heavy bleeding after 2 weeks, fever, or persistent tissue passage |
| Surgical abortion (in-clinic) | Immediate procedure-related cramping and light bleeding that decreases over days | Fever within days, increasing pain, or unusual discharge after initial recovery |
| Both types | Some spotting may last 2–4 weeks | Any fever ≥100.4°F, heavy bleeding metrics, or foul-smelling discharge |
Incomplete abortion is a more common cause of infection after medical abortion, while surgical procedures carry peri-procedural infection risk. The next sections describe procedure-specific warning signs.
Infection signs specific to medical abortion
Medical abortion uses mifepristone and misoprostol to cause the uterus to expel tissue over several days. Expect heavy bleeding and strong cramping at first that usually eases within a week. Signs of possible infection include bleeding that doesn’t settle after the expected timeframe, fever, foul-smelling discharge, or persistent pregnancy symptoms that suggest retained tissue. Because the process can be gradual, follow-up with ultrasound or serial hCG testing may be recommended if symptoms persist. If you have prolonged heavy bleeding, fever, or abnormal discharge more than a few days after the initial expulsion, contact your provider.
Next, surgical abortion risks and signs are covered.
Infection risks and signs after surgical abortion
Surgical abortion involves instruments placed in the uterus and is usually done in a single visit. Immediate cramping and light bleeding are common and normally improve over days. Infection can occur if bacteria are introduced during the procedure or if fragments are left behind, causing fever, localized pain, or smelly discharge within days. Some providers give prophylactic antibiotics in certain situations to reduce risk. If you develop fever, worsening pain, or unusual bleeding after a surgical abortion, seek prompt in-person evaluation to check for retained tissue, uterine perforation, or endometritis.
Knowing these differences helps you set expectations for follow-up and encourages timely care when red flags appear.
Complications that can lead to infection
Certain complications create conditions where bacteria can grow—retained products of conception (incomplete abortion), uterine perforation, or instrument-related injury are common examples. These issues leave necrotic tissue or change uterine anatomy, making infection more likely. If you notice ongoing bleeding, severe or persistent pain, or abnormal discharge, your provider may order an ultrasound to look for a complication.
The table below outlines common complications, typical signs, and usual diagnostic or treatment steps.
| Complication | Typical Signs | Diagnosis / Treatment Implication |
|---|---|---|
| Retained products of conception | Ongoing heavy bleeding, cramping, tissue passage, fever | Ultrasound evaluation; possible medical management or surgical evacuation (D&C) |
| Incomplete abortion | Continued pregnancy symptoms or rising hCG, persistent bleeding | Serial hCG or ultrasound; may require additional medication or procedure |
| Uterine perforation | Sudden severe pain, shoulder-tip pain, signs after instrumentation | Surgical assessment; possible repair and infection prevention |
| Procedural infection (endometritis) | Fever, foul discharge, pelvic tenderness | Clinical diagnosis; antibiotics and possible surgical removal of retained tissue |
How retained tissue or incomplete abortion leads to infection
Retained tissue provides dead material and blood where bacteria can multiply, causing uterine inflammation, ongoing bleeding, and foul discharge. You might suspect retained tissue if bleeding does not decrease, pain continues or worsens, or pregnancy tests stay positive longer than expected. Providers commonly use pelvic ultrasound to look for retained products and may use serial quantitative hCG measurements in some protocols. Treatment can range from expectant or medical management to surgical evacuation (D&C). Prompt care lowers the risk of wider infection and helps protect future fertility.
Signs of sepsis and when it’s an emergency
Sepsis is a life-threatening reaction to infection that needs immediate treatment. Red-flag signs include very high fever, very fast heart rate (tachycardia >100 bpm), low blood pressure or lightheadedness, rapid breathing, and changes in mental status. If you suspect sepsis, call emergency services and get to a hospital quickly—treatment usually requires IV antibiotics, fluids, and close monitoring. Early recognition and rapid treatment save lives, which is why prompt evaluation for post-abortion warning signs is so important.
Knowing sepsis criteria helps you act quickly if systemic symptoms appear.
When to seek immediate medical attention
Deciding whether to watch and wait, call your clinic, or go to the emergency department depends on measurable thresholds and how symptoms cluster. Seek immediate care for any of the following: fever ≥100.4°F with chills, heavy bleeding that meets pad metrics, fainting or near-fainting, severe unrelenting pelvic pain, or systemic signs of sepsis. For concerning but non-emergency symptoms—low-grade fever, increased bleeding without signs of low blood pressure, or new malodorous discharge—contact your provider the same day for triage. The checklist below helps you prioritize and tells you what to report when seeking care.
- Emergency (Go to ER / call emergency services): Unconsciousness, fainting, heavy bleeding (≥2 pads/hour × 2 hours), severe pain with lightheadedness, or sepsis signs.
- Urgent (Contact provider same day): Fever ≥100.4°F without collapse, foul-smelling discharge, increasingly heavy bleeding, or worsening pain.
- Non-urgent (Call for advice/monitor): Low-grade fever for <48 hours, mild increased cramping, or light spotting beyond expected duration.
This triage framework helps you choose the right level of care and leads into practical steps for contacting a healthcare team.
Urgent symptoms that need emergency care
Some symptoms can be immediately dangerous because they signal major blood loss or widespread infection. Urgent signs include passing large clots with dizziness, fainting, bleeding that soaks many pads quickly, severe abdominal pain with shock signs, or very high fever with confusion or trouble breathing. These conditions require fast stabilization in an emergency setting. If you have any of these signs, arrange safe transport and tell emergency staff your symptoms began after a recent abortion so they can triage and treat you appropriately.
Knowing these urgent thresholds reduces delays in life-saving treatment and prepares you to communicate clearly with providers.
How to decide when to contact your healthcare provider
If symptoms are concerning but not clearly life-threatening, follow a simple approach: check measurable thresholds (temperature, pads/hour), note how long it’s been since the procedure, and list any accompanying signs (odor, pain, dizziness). When you call, report exact temperature readings, how many pads you’ve soaked and over what time, the character of any discharge, and any systemic symptoms. This information helps triage nurses decide whether you need same-day evaluation, imaging, or immediate antibiotics. Many clinics offer telehealth triage to guide next steps—clear, objective reporting speeds up appropriate care and reduces worry.
If you prefer local in-person help, many community reproductive-health centers and regional clinics offer same-day triage, follow-up care, or referral to emergency services when needed.
How to prevent and manage post-abortion infections during recovery

Preventing infection combines simple hygiene, following your provider’s instructions, timely follow-up, and getting treatment if warning signs appear. These steps reduce bacterial growth and make it easier to spot retained tissue early. Key practices include washing hands before changing pads, avoiding intra-vaginal products or sex until cleared, finishing any prescribed medications, and attending scheduled follow-ups.
Practical steps to lower infection risk:
- Keep the genital area clean and change pads regularly; avoid douching or tampons until your provider says it’s safe.
- Rest and avoid heavy lifting for the timeframe your clinician recommends; follow any wound-care instructions.
- Finish any prescribed antibiotic course and attend follow-up appointments or telehealth checks.
- If indicated, get screened and treated for STIs, since co-infection can raise post-procedure infection risk.
These measures reduce the chance of infection and make it easier to notice problems early. Below is guidance on follow-up care.
Best practices to prevent infection after abortion
Prevention focuses on limiting bacterial exposure, confirming complete expulsion of tissue, and contacting care quickly if recovery changes. Practice strict hand hygiene, avoid internal vaginal devices or sex until cleared, and follow medication instructions carefully for medical abortion. Some clinicians recommend STI screening or prophylactic antibiotics in selected cases—discuss options with your provider. Regular follow-up, in person or by telehealth, helps confirm recovery and lets clinicians treat infection early if it develops.
Next, what to expect from proper post-abortion follow-up.
What proper post-abortion care and follow-up involve
Follow-up typically includes a check-in within 1–2 weeks to review bleeding, pain, and recovery. Your provider may do a pelvic exam, ultrasound, or serial pregnancy testing if needed. Telehealth visits are often used to triage symptoms and determine if in-person assessment is required; imaging is reserved for suspected retained tissue or persistent symptoms. If infection is suspected, clinicians will prescribe appropriate antibiotics and may arrange surgical management for retained tissue. Timely follow-up and treatment return most people to full health and reduce long-term risks.
Many community clinics and reproductive-health centers offer rapid follow-up, counseling, and referrals for in-person evaluation or medication management.
Frequently Asked Questions
If you have fever ≥100.4°F, heavy bleeding, foul-smelling discharge, or severe pelvic pain, seek medical attention promptly. For emergency signs like fainting, soaking through many pads quickly, or symptoms of sepsis, go to the emergency room right away. For worrying but non-emergency symptoms, call your healthcare provider the same day for guidance. Early care lowers the chance of complications. For more information on foul-smelling discharge, visit how to treat smelly discharge after abortion.
Normal recovery usually means cramping and bleeding that steadily improve. Infection may look like a persistent fever, heavy bleeding that soaks two or more pads per hour, foul-smelling discharge, or worsening pain. Use the measurable thresholds in this guide to help decide when to call for care.
Yes. Retained products of conception, pre-existing infections, or complications during the procedure (for example, uterine perforation) increase infection risk. Skipping post-procedure care instructions or poor hygiene can also raise the chance. Knowing these factors helps you take preventive steps and monitor recovery closely.
Follow-up lets providers confirm the uterus has emptied, check for symptoms that suggest infection, and treat problems early. A typical follow-up visit occurs within 1–2 weeks and may include an exam, ultrasound, or pregnancy testing. Early detection and treatment prevent worsening infection and protect health.
Yes. Good hygiene, changing pads regularly, avoiding douching or tampons until cleared, following post-abortion instructions, finishing prescribed medications, and attending follow-up visits all reduce infection risk. These steps help prevent bacterial growth and make complications easier to catch early.
Sepsis is a severe, life-threatening response to infection. Look for high fever, rapid heart rate, low blood pressure, confusion, or breathing difficulty. If you have these signs, seek emergency medical care immediately—early treatment is critical.
Yes. Medical abortions, which expel tissue over several days, can carry higher infection risk if tissue is retained. Surgical abortions may introduce bacteria during the procedure or leave fragments behind. Understanding these differences helps you know what to watch for and when to seek care.
How soon can infection develop after an abortion?
Infection can appear within days but sometimes surfaces weeks later; many cases show up in the first week when tissue or bacterial overgrowth causes inflammation. Factors that affect timing include retained tissue, pre-existing infection, or bacteria introduced during the procedure. Stay alert for fever, worsening pain, foul discharge, or heavy bleeding during the first few weeks and contact your provider if any occur.
Next: infection risk after medical abortion.
Can you get an infection after a medical abortion?
Yes. Most medical abortions proceed without infection, but there’s a small risk—especially if the abortion is incomplete or there was an existing infection. Watch for prolonged heavy bleeding, worsening pain, fever ≥100.4°F, or malodorous discharge. If you suspect infection after a medical abortion, contact your provider. Treatment may include antibiotics and, if needed, surgical evacuation.
Local reproductive-health centers and pregnancy-resource clinics can often provide follow-up, counseling, and arrange urgent care when infection is suspected.
Key takeaways:
- Watch measurable thresholds: fever ≥100.4°F, soaking ≥2 pads/hour ×2 hours, foul-smelling discharge.
- Act quickly: fever with systemic signs or heavy bleeding needs immediate care.
- Prevention helps: good hygiene, avoiding intra-vaginal activity until cleared, following medications, and attending follow-up reduce risk.
This FAQ reinforces the practical thresholds to use when deciding whether to seek care.
Conclusion
Knowing the warning signs of infection after an abortion helps you get care quickly and protect your health. Monitor clear thresholds—fever, heavy bleeding, and foul-smelling discharge—and contact your provider when symptoms meet the criteria in this guide. Simple prevention steps and timely follow-up reduce risk. If you’re unsure or worried, reach out to a local reproductive health clinic for advice and support.
Declaration
This article has been researched, written, and verified by the Smart Choice Team based on established medical guidelines and public health standards concerning post-abortion care.
Follow Us!