Birth Control Pill FAQ: Benefits, Risks, and How to Choose the Right Pill

The birth control pill is a daily oral hormonal contraceptive that prevents pregnancy by changing normal reproductive processes. This FAQ breaks down how pills work, the main formulations, benefits beyond pregnancy prevention, common side effects and rare but serious risks, and practical steps to match pill choices to your health goals and lifestyle. Many people want straightforward, evidence-based answers about effectiveness, side effects, drug interactions, and how to pick a pill that fits their medical history and routine. Here you’ll find clear explanations, comparison tables, and checklists you can use when talking with your clinician—covering mechanism of action, pill types, non-contraceptive benefits, safety considerations, and quick answers to common concerns like missed doses, mood changes, and weight.
What Are Birth Control Pills and How Do They Work?
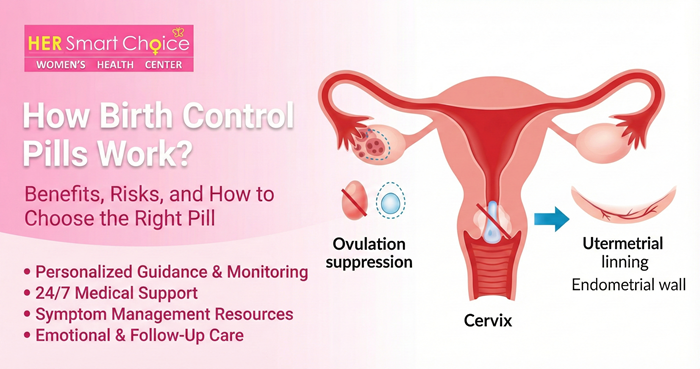
Birth control pills are oral medications that contain hormones—either both estrogen and a progestin (combined pills) or progestin alone (mini‑pills). They prevent pregnancy mainly by suppressing ovulation, thickening cervical mucus so sperm can’t reach an egg, and thinning the uterine lining to make implantation less likely. Combined and progestin‑only pills differ in hormone type and how sensitive they are to timing, which affects side effects and who can safely use them. Knowing these mechanisms explains why taking pills consistently and avoiding interacting medicines matters for effectiveness, and why certain health conditions rule out estrogen‑containing options. Our goal is to give clear, practical information so you can make confident, informed decisions about contraception.
What Hormones Are in Birth Control Pills and Their Roles?
Pills use two hormone classes: estrogen (commonly ethinyl estradiol) and synthetic progestins. Estrogen helps keep periods regular and supports ovulation suppression but also raises clotting risk in some people—an important factor when prescribing for smokers or older users. Progestins thicken cervical mucus to block sperm and thin the uterine lining; at higher doses or in certain formulations they may also suppress ovulation. Different progestins vary in androgenic or anti‑androgenic activity, which is why some pills can improve acne or influence mood differently from others. mood swings
How Do Birth Control Pills Prevent Pregnancy?
Pills reduce the chance of conception through three complementary actions. First, they suppress ovulation so an egg is not released. Second, they thicken cervical mucus, making it hard for sperm to move and survive. Third, they thin the endometrium, lowering the likelihood that a fertilized egg would implant. These layers of protection work best with correct use; missed pills, vomiting, diarrhea, or certain medications can weaken one or more mechanisms—so it’s important to know missed‑pill rules and interaction risks.
What Are the Different Types of Birth Control Pills?
Oral contraceptives fall into two main groups: combination pills (estrogen plus progestin) and progestin‑only pills. Within combination pills you’ll find monophasic formulations (same hormone dose each active pill), multiphasic packs (dose varies across the cycle), and extended‑cycle or continuous regimens that cut down or eliminate monthly withdrawal bleeds. Progestin‑only pills contain no estrogen and are often chosen for people who are breastfeeding or who have contraindications to estrogen, but they require stricter timing for reliable protection. Knowing these categories helps you match a clinical goal—acne control, lighter periods, breastfeeding compatibility—to the right formulation.
| Pill Type | Hormone Content / Cycle Type | Typical Use / Advantage |
|---|---|---|
| Monophasic combination | Estrogen + progestin; same dose daily | Simpler routine and predictable bleeding control |
| Multiphasic combination | Estrogen + progestin; varying doses across pack | Designed to mimic natural hormone shifts; may reduce some side effects for a few users |
| Extended-cycle combination | Estrogen + progestin; 91-day or continuous regimens | Fewer withdrawal bleeds—helpful for heavy periods or endometriosis |
| Progestin-only (mini-pill) | Progestin only; taken daily at the same time | Good for breastfeeding or estrogen contraindications; timing-sensitive |
This table summarizes how formulations differ and where they’re most useful—use it to narrow options before you talk with your clinician. Clear, practical information helps people choose a pill that fits both health needs and lifestyle.
What Are Combination Pills and Their Variations?
Combination pills pair estrogen with a progestin and come in monophasic, multiphasic, and extended‑cycle formats that change hormone exposure and bleeding patterns. Monophasic packs give a steady hormone dose each active day, which simplifies tracking side effects and cycle control. Multiphasic packs vary doses across the pack to more closely resemble natural fluctuations; some users find reduced breakthrough bleeding, though major advantages over monophasic pills are limited. Extended‑cycle regimens reduce or stop monthly withdrawal bleeds, which can improve quality of life for people with heavy periods or endometriosis.
What Are Progestin-Only Pills and Who Should Use Them?
Progestin‑only pills work mainly by thickening cervical mucus and, in some formulations, by suppressing ovulation. They’re a preferred option when estrogen is contraindicated—such as during breastfeeding or for people at higher clotting risk. A key limitation is strict timing: many mini‑pills must be taken within the same 3‑hour window each day to remain effective, so consistent routine and adherence are essential for dependable protection.
Progestin-Only Pills for Contraception: Efficacy and Acceptability This review compared progestin‑only oral contraceptives—administered continuously and without estrogen—to combined oral contraceptives. Randomized trials were examined to assess differences in effectiveness, acceptability, and continuation rates, but comparative conclusions remain limited by available data. Progestin‐only pills for contraception, 2010
A systematic review summarized continuous use of progestin‑only pills and highlighted the need for more head‑to‑head studies comparing them to combined options.
A New Progestin-Only Pill Containing Drospirenone: Efficacy and Safety Hormonal contraceptives are effective and generally safe for preventing pregnancy. Progestins are used in combined methods and as sole agents in progestin‑only pills, implants, intrauterine systems, and injections. Newer estrogen‑free progestin‑only formulations—such as a 4 mg drospirenone pill—offer ovulation inhibition with anti‑androgenic and anti‑mineralocorticoid actions and have been authorized in multiple regions. Oral progestins in hormonal contraception: importance and future perspectives of a new progestin only-pill containing 4 mg drospirenone, 2021
Recent progestin‑only options, including drospirenone formulations, expand estrogen‑free choices with promising efficacy and tolerability profiles.
What Are the Benefits of Taking Birth Control Pills?

Beyond strong contraceptive protection, birth control pills can improve everyday health and long‑term outcomes. They can make periods more predictable, ease menstrual cramps and reduce blood loss, help clear acne for many users, and treat conditions such as PCOS and endometriosis. Long‑term use is linked to lower ovarian and endometrial cancer risk, while evidence for other long‑term effects varies by formulation. Knowing how each benefit happens helps set realistic expectations for when and how much improvement to expect.
| Benefit | Mechanism | Typical Onset / Evidence Strength |
|---|---|---|
| Menstrual regulation | Hormone cycle control and endometrial stabilization | Weeks to months; strong clinical evidence |
| Reduced dysmenorrhea | Lower prostaglandin-driven bleeding and thinner lining | Weeks; moderate–strong evidence |
| Acne improvement | Anti‑androgenic progestins and reduced ovarian androgen production | 2–6 months; moderate evidence |
| Reduced ovarian/endometrial cancer | Suppressed ovulation and endometrial thinning | Years of use; strong epidemiological evidence |
The table ties each benefit to its hormonal mechanism and typical timeline, helping you weigh likely outcomes when choosing a pill.
How Effective Are Birth Control Pills at Preventing Pregnancy?
With perfect use, combination pills are about 99% effective; with typical use they’re closer to 91% because missed doses and timing lapses occur. “Perfect use” means taking the pill daily at the same time and avoiding interacting medications; “typical use” reflects real‑world adherence where missed pills and late doses reduce protection. Factors that lower effectiveness include missing multiple pills, taking enzyme‑inducing drugs, vomiting or prolonged diarrhea, and inconsistent timing for progestin‑only pills. Those numbers help explain why adherence and understanding interactions are so important.
What Non-Contraceptive Benefits Do Birth Control Pills Offer?
Many users gain symptom relief and longer‑term health advantages from hormonal contraception. Combined regimens and extended‑cycle options can reduce heavy or painful periods by limiting endometrial buildup. Pills with anti‑androgenic progestins commonly improve acne over several months. Epidemiological studies also show reduced ovarian and endometrial cancer risk with longer use—an important factor when weighing benefits against risks. These non‑contraceptive effects often guide the choice of formulation based on personal health goals.
Mechanism of Action of Progestin-Only Oral Contraceptives Progestin‑only oral contraceptives primarily prevent pregnancy by producing cervical mucus that is hostile to sperm, which reduces the chance of fertilization. This cervical mucus effect is a central mechanism for these agents. The mechanism of action of hormonal contraceptives and intrauterine contraceptive devices, 1999
For progestin‑only pills, the hostile cervical mucus is a key way they stop sperm from reaching an egg and thus prevent pregnancy.
What Are the Common Side Effects and Serious Risks of Birth Control Pills?
Most side effects are mild and improve within a few months as your body adjusts; serious complications are uncommon but important to recognize. Early side effects often include nausea, spotting between periods, breast tenderness, and short‑term headaches—many of which resolve after 2–3 cycles or after switching formulations. Rare but serious risks include venous thromboembolism (DVT or PE), stroke, and heart attack—risks that are mainly linked to estrogen‑containing pills in people with specific risk factors. Identifying higher‑risk individuals—like smokers over 35, people with a history of clots, or those with certain migraine types—helps guide safer prescribing.
Common side effects and basic management tips:
- Nausea: Try taking the pill with food or at bedtime; reassess after 1–2 cycles.
- Spotting or breakthrough bleeding: Often settles on its own; consider a different formulation if it persists beyond three cycles.
- Breast tenderness: Usually temporary; lower‑estrogen options may help if it continues.
- Headaches and mood changes: Track timing and severity; see a provider if symptoms are new, severe, or worsening to review options.
| Risk/Side Effect | Likelihood | Who’s at Higher Risk |
|---|---|---|
| Nausea, spotting, breast tenderness | Common; often transient | New users and those starting higher estrogen doses |
| Blood clots (DVT/PE) | Rare; combined pill ~3–9 per 10,000 woman‑years | Smokers >35, prior clot history, thrombophilia |
| Stroke / MI | Very rare in young healthy non‑smokers | Smokers, uncontrolled hypertension, older age |
| Cancer risks (breast/cervical) | Small absolute increase or neutral | Varies; benefits include reduced ovarian/endometrial risk |
Use this risk summary to guide a focused conversation with your clinician about which risks are most relevant to you.
What Are the Most Common Side Effects of Birth Control Pills?
Common side effects typically appear in the first few cycles and then often fade as hormone levels stabilize. Nausea usually improves with food or evening dosing; spotting or irregular bleeding often resolves after two to three cycles or when switching formulations. Breast tenderness and mild headaches are common and usually temporary. Mood effects vary—some users feel better, others notice worsening mood—so monitor changes closely during the first months and discuss alternatives with your provider if problems persist.
What Serious Health Risks Are Associated with Birth Control Pills?
Serious risks are uncommon but clinically meaningful. Estrogen‑containing pills raise the relative risk of venous thromboembolism, but the absolute risk remains low for most young, healthy, non‑smokers. The greatest increases in clot risk occur in smokers over 35 and people with a personal or strong family history of clotting disorders; these groups are often advised to avoid combined pills. Stroke and heart attack are rare in young healthy individuals but rise with traditional cardiovascular risk factors like hypertension, smoking, and older age. The cancer risk profile is mixed: ovarian and endometrial cancer risk is reduced with pill use, while small, variable effects on breast and cervical cancer have been reported—these trade‑offs should be discussed individually with a clinician.
How Do You Choose the Right Birth Control Pill for Your Needs?
Choosing the right pill means matching your medical history, lifestyle, and health priorities to pill characteristics in a clear, patient‑centered way. Start by listing absolute and relative contraindications—smoking status, age, clotting history, migraines with aura, and blood pressure—that may rule out estrogen‑containing options. Then align goals (acne control, fewer periods, breastfeeding) with pill types: anti‑androgenic combination pills for acne, extended‑cycle regimens for heavy or painful periods, and progestin‑only options when estrogen isn’t appropriate. This process helps prepare for a productive shared decision with your clinician.
Decision checklist (begin here when preparing to consult a clinician):
- Medical contraindications: Note smoking status, age, any clotting history, migraine type, and blood pressure.
- Lifestyle factors: Consider your ability to take a daily pill on time, desire for fewer periods, and breastfeeding plans.
- Health goals: Prioritize acne reduction, menstrual control, PCOS management, or minimizing side effects.
- Medication review: List enzyme‑inducing drugs or other medicines that could lower contraceptive levels and discuss alternatives.
This checklist supports shared decision‑making with your provider and highlights safety and adherence factors that usually determine the best option.
What Medical and Lifestyle Factors Affect Birth Control Pill Choice?
Several medical and lifestyle details guide which pill is safest and most effective for you. Key medical factors include prior blood clots, smoking combined with age over 35, uncontrolled hypertension, and migraine with aura—conditions that typically rule out estrogen‑containing pills. Lifestyle factors include whether you can take a pill at the same time every day (especially important for progestin‑only pills), travel or work schedules that affect timing, and whether you want to reduce or skip monthly bleeding. Medication interactions—particularly enzyme‑inducing drugs—can lower hormone levels, so a full medication review is essential when selecting an oral contraceptive.
How Do Specific Health Goals Influence Pill Selection?
Your specific goals point to formulations most likely to deliver the desired results. For acne, combined pills with anti‑androgenic progestins are often effective. For heavy periods or endometriosis, extended‑cycle or continuous regimens reduce endometrial growth and bleeding. If you’re breastfeeding or have an estrogen contraindication, progestin‑only options provide contraception without estrogen exposure and with minimal effect on milk supply. When cardiovascular risk is a concern—because of smoking or age—non‑estrogen methods or long‑acting reversible contraception may be safer, so individualized counseling is important.
What Are the Most Frequently Asked Questions About Birth Control Pills?
Below are concise, practical answers to common concerns—missed pills, weight and mood effects, stopping the pill, and interactions—so you can act quickly and know when to seek clinical help. Short, evidence‑based answers help you find reliable guidance and plan follow‑up with your clinician when needed.
What Should You Do If You Miss a Birth Control Pill?
Steps depend on the pill type and how many doses were missed. For combination pills: if you miss one active pill, take it as soon as you remember and continue the pack; if you miss two or more, follow the specific instructions on your pack, use backup contraception, and consider emergency contraception depending on timing and unprotected sex. For progestin‑only pills: a dose taken outside the strict timing window (usually more than 3 hours late) should be taken right away, and you should use condoms for 48 hours; consider emergency contraception if you had unprotected intercourse during the risk window. When unsure, treat the situation as higher risk: use condoms, consult a provider, and consider emergency contraception if appropriate.
Can Birth Control Pills Cause Weight Gain or Mood Changes?
Evidence shows little consistent link between modern birth control pills and significant weight gain for most users, though individual experiences vary and lifestyle factors can play a role. Mood effects are individual: some people note worsened mood or depressive symptoms with certain formulations, while others feel no change or even improvement. Monitor weight and mood during the first few cycles; if changes are meaningful or persistent, talk with your clinician about trying a different progestin, adjusting the formulation, or switching to a non‑hormonal method. Open monitoring and communication help tailor choices to your wellbeing.
Our aim is to give clear, user‑friendly answers about the benefits, risks, and options for birth control pills so you can make informed choices and feel confident discussing options with your healthcare provider.
Conclusion
Knowing the benefits and risks of birth control pills helps you choose a method that fits your health needs and lifestyle. Pills can regulate cycles, ease symptoms, and lower certain long‑term cancer risks, but they also carry side effects and contraindications that require careful consideration. Talk through your personal health goals and risk factors with a healthcare provider to find the right formulation or alternative method. When you’re ready, explore our resources and connect with a clinician to take the next step in your reproductive health journey.










